For years, treating type 2 diabetes meant one thing: lower blood sugar. But today, the game has changed. A new class of drugs called SGLT2 inhibitors isn’t just helping people control their glucose-it’s saving hearts and kidneys too. If you or someone you know has type 2 diabetes, especially with heart or kidney issues, this isn’t just another pill. It’s a turning point in how we manage the disease.
What Are SGLT2 Inhibitors?
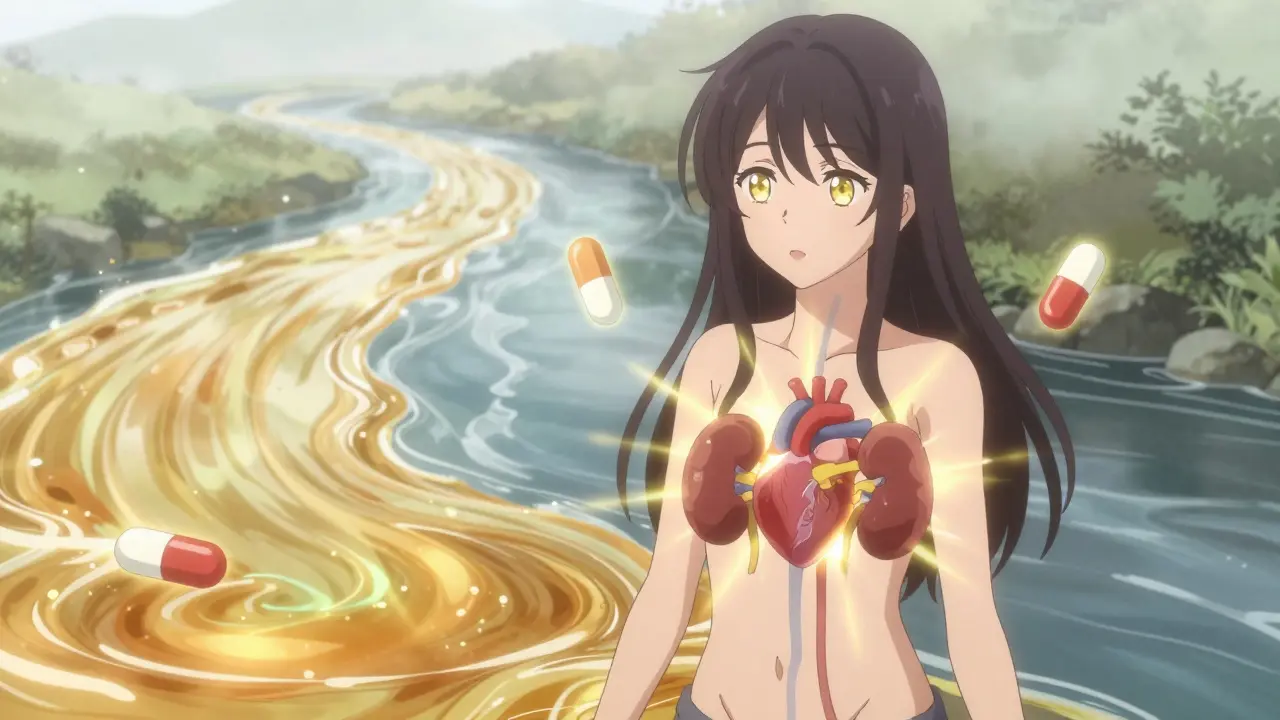
SGLT2 inhibitors-also known as gliflozins-are oral medications that work in your kidneys, not your pancreas. Unlike insulin or metformin, they don’t rely on your body’s ability to produce or respond to insulin. Instead, they block a protein in your kidneys called SGLT2, which normally reabsorbs glucose back into your blood. When you take one of these drugs, your body simply pees out the extra sugar.
That’s it. No fancy tricks. Just a natural process you’re nudging. The result? Lower blood sugar, modest weight loss (usually 2-3 kg), and a small but meaningful drop in blood pressure. Common brands include Jardiance (empagliflozin), Farxiga (dapagliflozin), Invokana (canagliflozin), and Steglatro (ertugliflozin). All taken once a day, usually in the morning.
They were first approved in the U.S. starting in 2013. But no one expected what came next.
The Big Surprise: Heart Protection
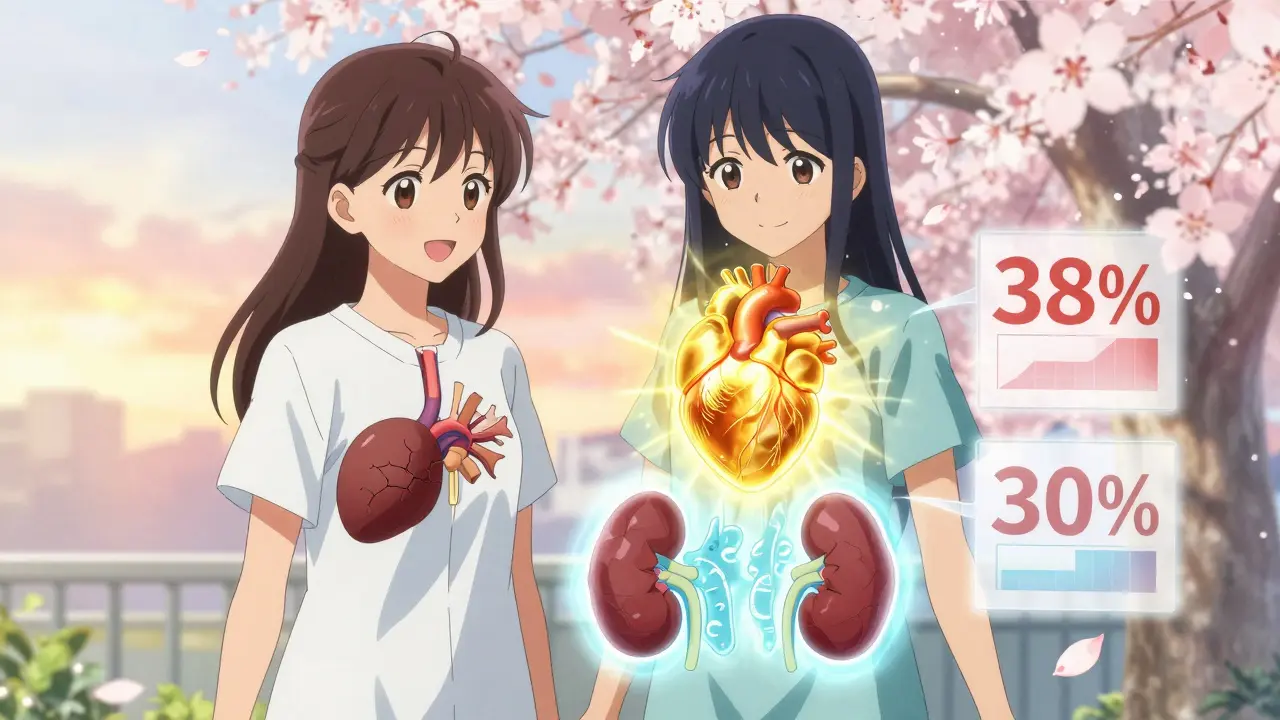
In 2015, a study called EMPA-REG OUTCOME changed everything. Researchers gave empagliflozin to people with type 2 diabetes and known heart disease. The goal? See if it lowered blood sugar. What they found stunned the medical world: those taking empagliflozin had a 38% lower risk of dying from heart-related causes. Their risk of dying from any cause dropped by 32%.
That wasn’t a fluke. Other trials followed. CANVAS showed canagliflozin reduced heart attacks, strokes, and heart-related deaths by 14%. DECLARE-TIMI 58 confirmed these benefits across broader groups. And here’s the kicker: these drugs worked even in people whose blood sugar didn’t improve much. The benefit wasn’t just about glucose-it was about the heart itself.
By 2022, the American Heart Association updated its guidelines to recommend SGLT2 inhibitors for all patients with heart failure-even if they don’t have diabetes. Why? Because DAPA-HF and EMPEROR-Reduced trials showed these drugs cut hospitalizations for heart failure by 25-30%. One patient on Reddit said, “My ejection fraction went from 25% to 35% after starting Farxiga. My cardiologist said it was remarkable.”
Kidney Benefits: Slowing Down Damage
Diabetes is the leading cause of kidney failure. For years, doctors had few tools to stop it. Then came CREDENCE. This trial focused on people with type 2 diabetes and early kidney damage. Those taking canagliflozin had a 30% lower risk of ending up on dialysis, needing a transplant, or dying from kidney disease.
That’s huge. And it wasn’t just about sugar. The drugs reduce pressure inside the kidney’s filtering units (glomeruli), which slows long-term damage. Even if your blood sugar is under control, SGLT2 inhibitors still help your kidneys. The EMPA-KIDNEY trial in 2023 showed the same benefit in people with chronic kidney disease-even without diabetes. That’s why the FDA approved dapagliflozin for CKD in 2021, regardless of diabetes status.
Doctors now use these drugs not just to treat diabetes, but to protect kidneys in high-risk patients. The American Society of Nephrology recommends starting them when urine albumin levels are elevated, even before kidney function drops.
How Do They Compare to Other Diabetes Drugs?
Metformin is still the first-line drug. It’s cheap, safe, and helps with weight. But it doesn’t reduce heart attacks or kidney failure like SGLT2 inhibitors do. Sulfonylureas? They lower sugar but cause low blood sugar and weight gain. DPP-4 inhibitors like sitagliptin? They’re neutral on heart and kidney risk.
Here’s a quick comparison:
| Medication | Cost (Monthly) | HbA1c Reduction | Heart Benefit | Kidney Benefit | Weight Change |
|---|---|---|---|---|---|
| Metformin | $4 | 0.5-1.0% | Minimal | None proven | Neutral |
| Sulfonylureas | $10-15 | 0.5-1.5% | No | No | Gain |
| DPP-4 Inhibitors | $350-400 | 0.5-0.8% | Neutral | Neutral | Neutral |
| SGLT2 Inhibitors | $520-600 | 0.5-1.0% | Yes | Yes | Loss (2-3 kg) |
The cost is higher, but for people with heart or kidney disease, the long-term savings-fewer hospital stays, less dialysis, fewer emergency visits-make it worth it. One study found SGLT2 inhibitors cost less than $38,400 per quality-adjusted life year gained, well below the $50,000 benchmark for cost-effectiveness in the U.S.
Side Effects and Risks
Nothing’s perfect. The most common side effects are genital yeast infections-about 4-5% of users, mostly women. Urinating more often is also common, especially at first. Some people say it’s annoying, but it usually settles down.
The bigger concern is diabetic ketoacidosis (DKA). It’s rare-only 0.1-0.3% of users-but it can happen even when blood sugar isn’t very high. This is called “euglycemic DKA.” If you’re sick, fasting, or having surgery, talk to your doctor. You might need to pause the drug temporarily.
Canagliflozin has a small increased risk of leg amputations-about 6.3 events per 1,000 patients per year. That’s why doctors avoid it in people with poor circulation or foot ulcers.
These drugs aren’t for everyone. They’re not approved for type 1 diabetes. And if your kidney function is too low (eGFR below 30), they won’t work. Most doctors start them only if your eGFR is above 45.
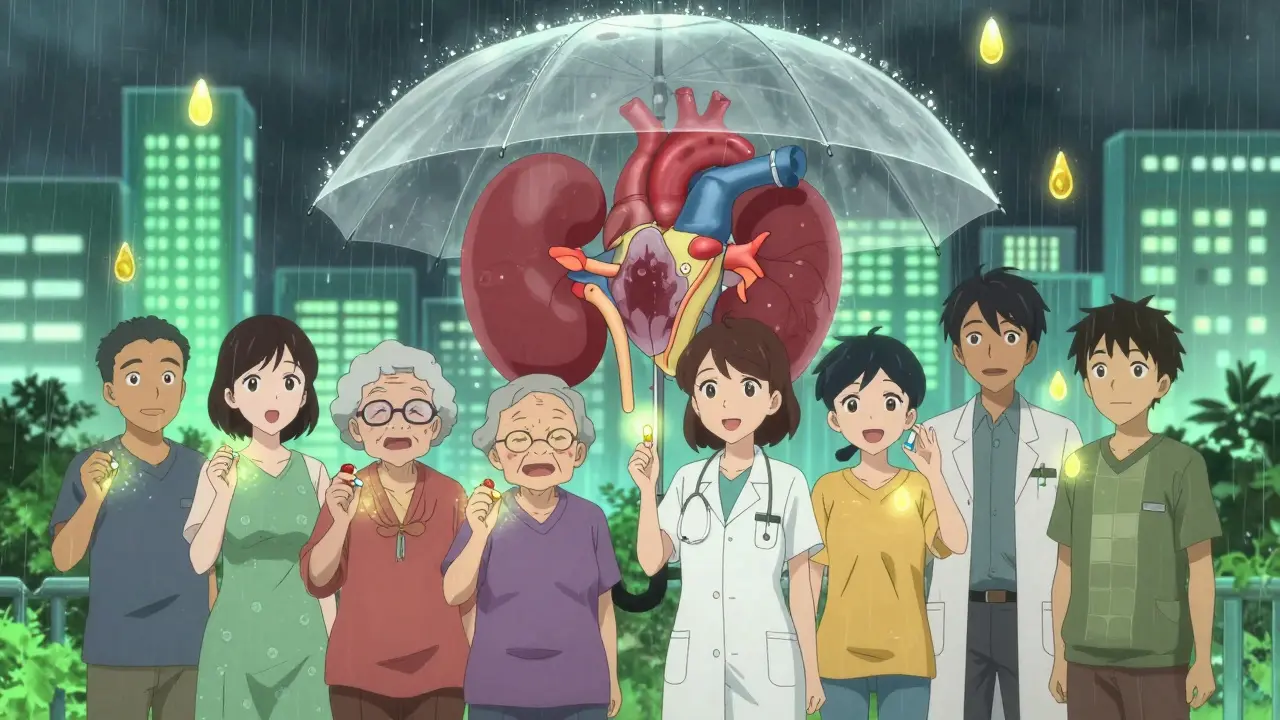
Who Should Be Taking Them?
Based on guidelines from the American Diabetes Association and European Society of Cardiology, SGLT2 inhibitors are now first-choice for:
- People with type 2 diabetes and heart failure
- Those with chronic kidney disease (even without diabetes)
- Patients with a history of heart attack or stroke
- Anyone with high blood pressure and protein in their urine
If you have diabetes but no heart or kidney issues yet, these drugs aren’t usually the first pick. Metformin still wins there. But if you’re at risk-say, you’re overweight, have high blood pressure, or your A1c is creeping up-starting an SGLT2 inhibitor early might prevent problems down the road.
What to Expect When You Start
When you begin, your doctor will check your kidney function and blood pressure. You might notice:
- More trips to the bathroom (especially at night at first)
- Lightweight feeling-some lose 2-5 pounds in the first week from water loss
- A slight dip in eGFR (kidney function number) after a few weeks. This is normal. It’s not damage-it’s your kidneys adjusting to less pressure.
Your doctor will likely recheck your kidney function in 4-6 weeks. If it drops more than 30%, they’ll investigate. But if it stabilizes? That’s a good sign.
Don’t stop the drug if you get a yeast infection. It’s treatable. But do tell your doctor. And if you feel nauseous, dizzy, or unusually tired during illness-call your provider. You might need to pause the medication.
The Future: What’s Next?
Research is moving fast. Trials are now testing SGLT2 inhibitors in prediabetes, obesity without diabetes, and even non-alcoholic fatty liver disease. Early data suggests they may slow liver scarring and reduce fat buildup in the liver.
Generic versions are coming. Patents for Jardiance and Farxiga expire between 2025 and 2028. Prices could drop by 60-70%. That’ll make these life-saving drugs accessible to far more people.
By 2027, the global market for these drugs is expected to hit $18.5 billion. Why? Because doctors now see them not as diabetes pills-but as heart and kidney protectors. And that’s a big shift.
Do SGLT2 inhibitors cause low blood sugar?
Not usually-unless you’re also taking insulin or sulfonylureas. SGLT2 inhibitors work independently of insulin, so they rarely cause hypoglycemia on their own. That’s one reason they’re safer than older drugs like glipizide or glyburide.
Can I take SGLT2 inhibitors if I have kidney disease?
Yes-if your kidney function isn’t too low. Most can be used safely if your eGFR is above 30. Some, like dapagliflozin, are approved for use even in advanced kidney disease (eGFR as low as 25). But they’re not used if your eGFR is below 20-25, depending on the drug. Always check with your doctor.
Why do SGLT2 inhibitors help the heart if they’re kidney drugs?
It’s not fully understood, but experts believe it’s about reducing pressure and inflammation. By making your kidneys excrete more sodium and water, they lower blood pressure and reduce fluid overload on the heart. They may also improve how the heart uses fuel-switching from sugar to ketones, which is more efficient. These changes help the heart pump better and recover from damage.
Are SGLT2 inhibitors safe for older adults?
Yes, but with caution. Older adults are more prone to dehydration and low blood pressure. Doctors often start with a lower dose and monitor closely. If you’re on diuretics or have a history of falls, your doctor will weigh the benefits against the risk of dizziness or fainting.
How long does it take to see benefits?
Blood sugar drops in days. Weight loss and lower blood pressure show up in 2-4 weeks. But the real benefits-fewer heart attacks, slower kidney decline-take months or years to show up in studies. That’s why doctors say: start early, stay consistent.
Final Thoughts
SGLT2 inhibitors aren’t magic. They don’t cure diabetes. But they’ve changed how we think about it. This isn’t just about sugar anymore. It’s about protecting your most vital organs. If you have type 2 diabetes and heart or kidney issues, asking your doctor about these drugs isn’t optional-it’s essential. The evidence is clear. For many, they’re the most important medicine they’ll ever take.





Comments (9)
Elaine Douglass
I started Jardiance last year after my heart failure diagnosis and honestly it changed everything
My energy came back and my doctor said my ejection fraction improved
I used to be terrified to walk to the mailbox now I walk two miles most days
Yeah the bathroom trips were rough at first but my body adjusted
And no more scary low sugar episodes like I had with the old meds
It’s not magic but it’s the closest thing I’ve felt in years
Takeysha Turnquest
We treat diabetes like a number when it’s really a symphony of broken systems
These drugs don’t fix glucose they reharmonize the body’s rhythm
They whisper to the kidneys and the heart listens
And for the first time in decades medicine isn’t just chasing sugar
It’s listening to what the organs are screaming to say
Alex Curran
Just want to clarify something I see a lot of confusion about
The eGFR dip you see early on isn’t kidney damage it’s the drug reducing intraglomerular pressure
It’s actually protective long term
Think of it like lowering the pressure in a leaky pipe so it doesn’t burst
Doctors should explain this better because patients panic when they see the lab numbers drop
And yes I’m a nephrologist in Sydney and I’ve prescribed these to over 200 patients
Dikshita Mehta
My mom has CKD and type 2 diabetes and we started her on dapagliflozin six months ago
Her albumin levels dropped by 40% and her BP is more stable
She still gets yeast infections but we manage them with probiotics and cranberry
It’s not perfect but it’s the first treatment that actually slowed her kidney decline
I wish more people knew this wasn’t just a diabetes drug
It’s a kidney shield
pascal pantel
Let’s be real the entire SGLT2 hype is just pharma’s clever rebranding
They took a glucosuria-inducing diuretic and slapped on a cardiovascular benefit because they needed a new blockbuster
Yes the trials show statistical significance but the absolute risk reduction is tiny
And the cost is absurd when metformin costs four bucks
Also euglycemic DKA is terrifying and underreported
And don’t even get me started on the amputation risk with canagliflozin
This is medicine being sold as miracle tech when it’s just a slightly better diuretic
Gloria Parraz
If you’re reading this and you have diabetes with heart or kidney issues
Don’t wait for your doctor to bring it up
Ask for an SGLT2 inhibitor
It’s not about being aggressive it’s about being informed
I’ve seen too many people suffer avoidable hospitalizations because they didn’t know
These aren’t just pills they’re time machines
They give you back years you didn’t know you were losing
Start the conversation today
Sahil jassy
Been on Farxiga for 18 months
Lost 6 lbs naturally no dieting
My BP dropped from 145/90 to 122/78
And my kidney doc says my GFR stabilized
Yeast infection once but used clotrimazole and it vanished
Worth every penny
Also I’m from India and these drugs are still unaffordable here
Hope generics come soon
Kathryn Featherstone
I’m a nurse and I’ve watched patients transform on these drugs
One man came in for his first follow-up looking defeated
Three months later he walked in smiling holding his grandkids
He said he finally felt like himself again
It’s not just the numbers it’s the dignity they restore
These drugs don’t just treat disease they give life back
Nicole Rutherford
Everyone’s acting like this is groundbreaking when it’s just another bandaid
You still have to watch your diet and exercise
And you’re still diabetic
And the side effects are annoying and sometimes dangerous
And the cost is insane
And if you don’t have heart or kidney disease you’re wasting your money
Stop treating this like a miracle and start treating it like a tool
And maybe stop letting pharma dictate your treatment