When you're about to write a prescription, the last thing you want is for your patient to walk out of the office only to find out their insurance won't cover the drug - or worse, they’ll pay $200 for a pill that costs $8 at another pharmacy. This isn’t just a billing problem. It’s a care problem. And it happens more often than most providers admit.
That’s why checking the formulary - also called a Preferred Drug List (PDL) - before prescribing isn’t optional. It’s essential. Formularies are the lists of medications covered by a patient’s health plan. They’re not random. Every drug on the list has been reviewed by doctors and pharmacists for safety, effectiveness, and cost. But here’s the catch: these lists change. Often. And they vary wildly between insurers, plans, and even states.
What Exactly Is a Formulary?
A formulary is a dynamic, tiered list of drugs approved by a health plan. It’s built by a Pharmacy and Therapeutics (P&T) committee - a group of clinicians who review clinical data, real-world outcomes, and cost trends. For example, HealthPartners updates its Medicare formulary four times a year: January, April, July, and October. These aren’t minor tweaks. They’re full reevaluations based on new FDA approvals, generic competition, and budget impacts.
Medicare Part D plans, which cover over 50 million Americans, must follow strict CMS rules. They must include at least two drugs per therapeutic category and offer an exceptions process. Commercial plans? They have more flexibility. UnitedHealthcare uses a four-tier system. Aetna uses five. Medicaid programs vary by state - 42 states have closed formularies, meaning you need prior authorization just to prescribe a drug not on the list.
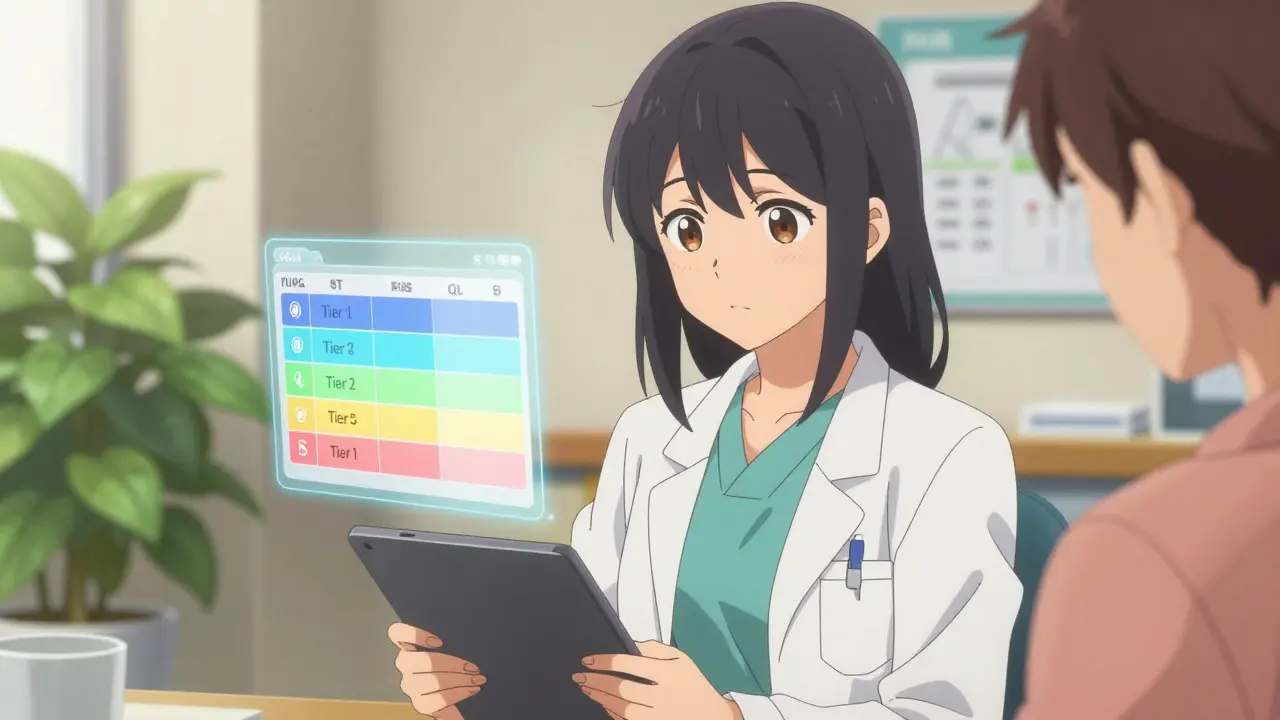
Each drug on the formulary comes with codes that tell you what hurdles stand between the prescription pad and the pharmacy counter:
- PA = Prior Authorization - you need to submit paperwork before the drug is approved.
- ST = Step Therapy - the patient must try and fail on a cheaper drug first.
- QL = Quantity Limit - you can’t prescribe more than X pills per month.
Missing one of these? You’re setting up your patient for a surprise at the pharmacy.
How Tiers Drive Out-of-Pocket Costs
Formularies aren’t just lists. They’re pricing engines. Most use 3 to 5 tiers, and each tier changes how much the patient pays.
Take a typical Medicare Part D plan in 2024:
- Tier 1: Preferred generics - $1 to $5 per prescription. Think metformin, lisinopril, atorvastatin.
- Tier 2: Non-preferred generics - $10 to $20.
- Tier 3: Preferred brands - $30 to $50. These are newer, clinically superior brands like Januvia or Eliquis.
- Tier 4: Non-preferred brands - $60 to $100. Often older brands with cheaper generic alternatives.
- Tier 5: Specialty drugs - $950+ per month. Patients pay 25% coinsurance. Think cancer therapies or rare disease treatments.
That’s not theoretical. In Portland, a patient on a Medicare plan paid $92 for a 30-day supply of a Tier 4 brand-name drug - but only $4 for the same medication in Tier 1. The difference? A single formulary check.
Where and How to Check Formularies
You have three main ways to check a formulary - and you should use all of them.
1. Insurer Websites
Most insurers have searchable drug lists. Aetna, UnitedHealthcare, and Excellus BCBS all offer tools where you enter the drug name, patient’s county, and plan name. These tools flag PA, ST, and QL requirements in real time.
Pro tip: Bookmark the direct link to the 2024 formulary page for each major insurer you work with. For example:
- UnitedHealthcare: uhc.com/medicare/drug-list
- Aetna: aetna.com/medicare/drug-list
- Excellus BCBS: excellusbcbs.com/medicare/formulary
These links change yearly. Always verify you’re on the current year’s page.
2. EHR-Integrated Tools
Large health systems - like Kaiser, Northwestern Medicine, or Mayo Clinic - embed formulary checkers directly into their electronic health records (EHR). Epic’s Formulary Check module, for example, shows real-time tier status and prior authorization needs as you type a prescription. Northwestern Medicine cut prescription abandonment by 42% after rolling this out in Q3 2023.
If your clinic uses Epic, Cerner, or Allscripts, ask your IT team if formulary integration is enabled. If not, push for it. This isn’t a luxury - it’s a safety net.
3. CMS Plan Finder
For Medicare patients, the Medicare Plan Finder covers 99.8% of Part D plans. You can search by drug name, zip code, and plan type. It shows estimated monthly costs and whether the drug is on formulary. Use this when a patient switches plans mid-year - which happens to 28% of beneficiaries, according to the GAO.
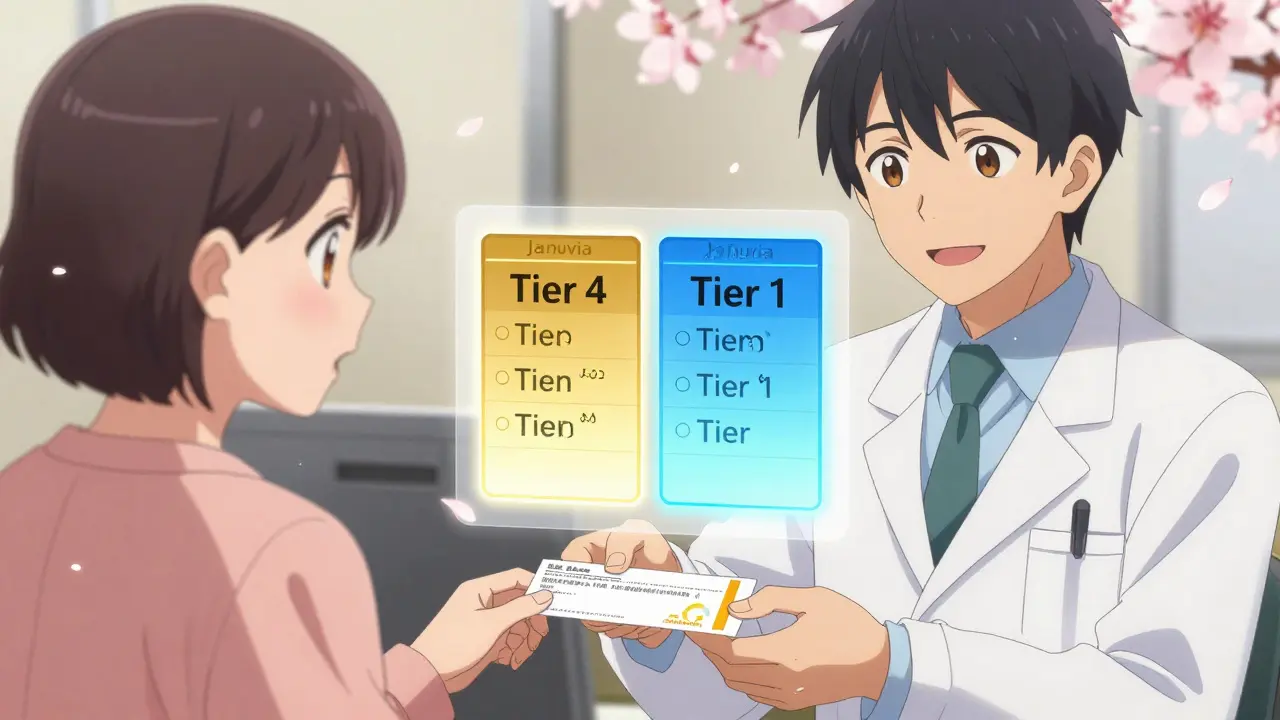
Why Formularies Vary So Much - And Why It Matters
One drug, three different rules. That’s not a glitch. That’s the system.
Take Januvia. In one Medicare plan, it’s Tier 3 with no restrictions. In another, it’s Tier 4 with step therapy. In a third, it’s not covered at all - and the patient must switch to a generic. A Reddit post from October 2024 sums it up: “Three different Medicare formularies in my practice each classify Januvia differently. I have to check each patient’s plan before prescribing.”
This isn’t just frustrating. It’s dangerous. A February 2024 AMA report found that 34% of prior authorization delays led to serious adverse events - like uncontrolled diabetes or hospitalization for heart failure. The average primary care provider spends 18.7 minutes per patient just verifying coverage. That’s over 3 hours a week per clinician.
What’s Changing in 2025 and Beyond
The Inflation Reduction Act’s $2,000 annual out-of-pocket cap for Medicare Part D kicks in January 2025. That’s already reshaping formularies. Avalere Projected that 73% of 2025 Medicare formularies are moving more drugs to lower tiers to reduce patient costs.
Also, by January 1, 2026, CMS requires all Medicare Part D plans to implement Real-Time Benefit Tools (RTBT). This means formulary and cost data will auto-populate into your EHR as you write the script - no more manual checks. Epic’s FormularyAI, launched in August 2024, already predicts coverage likelihood with 87% accuracy by analyzing 10 million historical prior auth decisions.
But don’t wait. RTBT isn’t here yet. And even when it is, you’ll still need to know how to read a formulary manually. Because not every patient is on Medicare. Not every insurer has RTBT. And not every prescription is written in a big health system.
Practical Workflow: How to Do This Every Time
Here’s a simple routine that takes less than 60 seconds per patient:
- When selecting a drug, pause. Ask: “Is this on formulary?”
- Check the insurer’s website or EHR tool. Look for PA, ST, or QL flags.
- If the drug isn’t covered, ask: “Is there a Tier 1 or 2 alternative?”
- If no alternative exists, initiate prior authorization immediately - don’t wait for the patient to get to the pharmacy.
- Document the decision in the chart: “Formulary checked: Tier 3, no restrictions. Patient advised of cost.”
Set calendar reminders for quarterly formulary updates. Subscribe to your insurer’s provider alerts. Keep printed formularies in your office if you work in a rural clinic - 41% of rural providers still do.
What Happens When You Don’t Check
Patients abandon prescriptions. One study found 27% of patients skip filling a new script because of cost surprises. That’s not just lost revenue - it’s worse health outcomes. Uncontrolled hypertension. Missed insulin doses. Hospital readmissions.
And you? You lose trust. Patients don’t blame the insurance company. They blame you. “You prescribed this. Why didn’t you know it wouldn’t work?”
Formulary checks aren’t paperwork. They’re part of clinical judgment. Just like checking for allergies or drug interactions.
How often do formularies change?
Formularies update at least quarterly, with Medicare Part D plans required to notify patients 60 days before any negative change. Many insurers like HealthPartners publish updates in January, April, July, and October. Some plans make mid-year adjustments if a drug is recalled, a generic enters the market, or costs spike unexpectedly.
Can I prescribe a drug not on the formulary?
Yes - but it’s not easy. For closed formularies (common in Medicaid), you must submit a prior authorization request explaining why the non-formulary drug is medically necessary. For Medicare Part D, plans must grant exceptions within 72 hours (24 hours for urgent cases). If denied, you can appeal. But delays can harm patients - especially in cancer or mental health care.
Do all insurers use the same tiers?
No. Medicare Part D plans must use five tiers. Commercial plans vary: UnitedHealthcare uses four, while some Medicaid programs use three. The cost structure differs too - a Tier 3 brand-name drug might cost $40 on one plan and $80 on another. Always check the specific plan’s formulary, not just the insurer’s name.
What if my patient is on Medicaid?
Medicaid formularies are state-specific. For example, Minnesota uses a single PDL for all state-funded plans, while Texas has separate lists for different Medicaid programs. Check your state’s Department of Health website. Most states publish their Preferred Drug List online. Some require prior authorization for even generic drugs.
Are there tools that automate this?
Yes. Epic, Cerner, and Allscripts now integrate formulary data into EHRs. By 2026, CMS requires all Medicare Part D plans to offer real-time benefit tools that push formulary and cost info directly into your prescribing workflow. But until then, manual checks are still necessary - especially for patients on commercial plans or those with complex coverage.
Final Thought: This Is Clinical Work
Checking a formulary isn’t administrative busywork. It’s part of prescribing. You wouldn’t prescribe a beta-blocker to someone with asthma without checking contraindications. Don’t prescribe a $90 drug without checking if it’s covered - or if a $5 alternative exists.
The system is broken. But you’re still the gatekeeper. And every time you check a formulary, you’re not just saving money. You’re preventing delays, hospitalizations, and broken trust. Do it every time. No exceptions.