
Every year, over 60,000 children under age 6 end up in emergency rooms because they got into medications stored improperly at home. That’s not a rare accident-it’s a predictable outcome of how most families keep their medicine. A simple medication storage checklist can cut those numbers by nearly 90%. It’s not about being paranoid. It’s about making sure your pills, patches, and inhalers don’t become hazards to your kids, pets, or even yourself when you’re tired or confused.
Where Not to Store Your Medications
The bathroom cabinet is the worst place in your house for medicine. Why? Showers turn it into a steam room. Humidity spikes to 80-90%, temperatures jump 10-15 degrees, and light floods in every time you open the door. That’s exactly what degrades pills. Studies show some medications lose up to 50% of their strength in just a few months under those conditions. Even your kitchen near the stove or a sunny windowsill is a bad idea. Heat and light break down active ingredients faster than you think.
Instead, pick a cool, dry, dark spot that’s out of daily sight. A locked closet in a hallway, a high shelf in a bedroom dresser, or a dedicated cabinet in a rarely used room works best. The goal isn’t convenience-it’s isolation. If your kids don’t think to look there, they won’t find it.
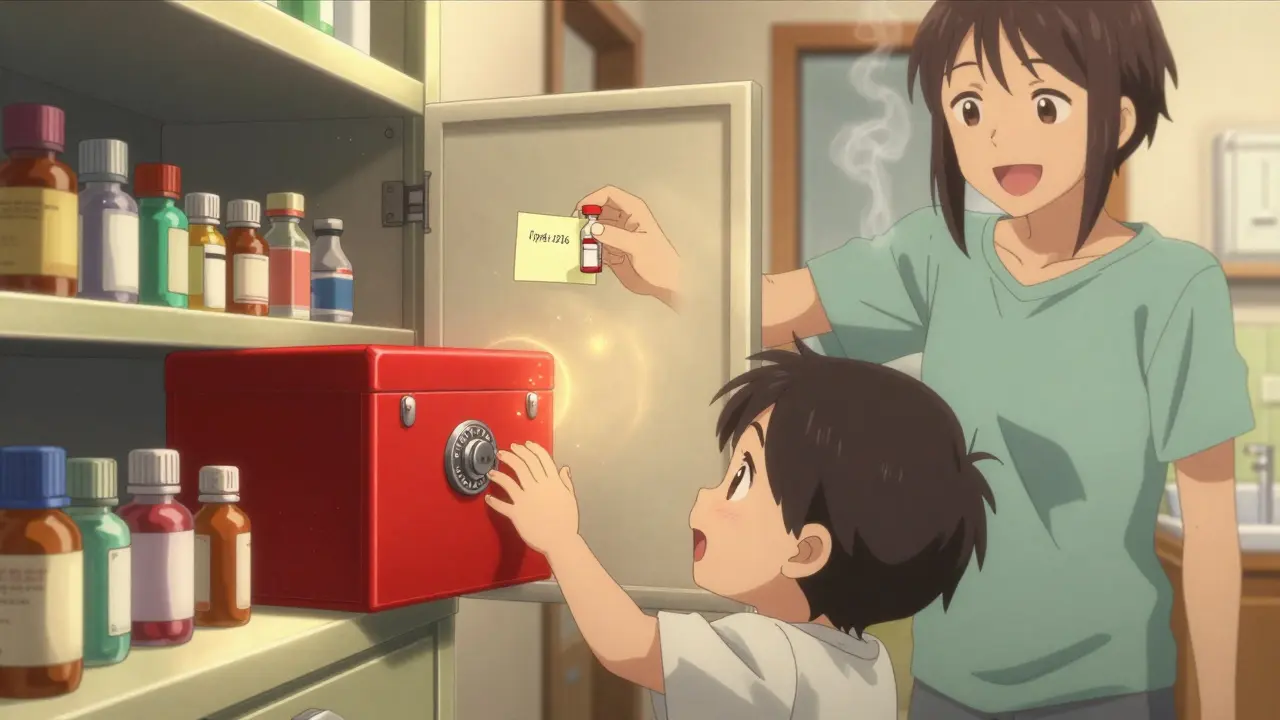
Lock It Down-No Exceptions
Standard medicine cabinets? They’re basically decorative. The Consumer Product Safety Commission tested them and found they stop only 12% of kids from getting inside. That’s not safety-it’s luck. If you have children, grandchildren, teens, or anyone who might wander into your medicine drawer, you need a lock.
Look for a small, affordable medicine lockbox with a combination lock. They’re cheaper than a coffee maker and far more important. A 2023 Pediatrics study showed households using lockboxes saw 92% fewer accidental ingestions by children under five. Key locks? Less reliable-kids can find keys. Combination locks? You set the code, and if you forget it, you reset it. Avoid anything with a simple slide latch. If it can be opened with a butter knife, it’s not secure.
And if you have opioids, insulin, or other high-alert medications? Double lock them. One lock on the box, another on the cabinet or drawer it sits in. This isn’t overkill-it’s what hospitals do for a reason.
Separate, Label, and Sort
Imagine this: You’re rushing in the morning. You grab what looks like your blood pressure pill-but it’s your husband’s warfarin. That’s not a mistake you recover from. That’s why every medication must be stored separately.
Use separate bins, drawers, or even just different sides of a shelf. No mixing prescriptions. No piling OTC painkillers on top of your thyroid pills. The Institute for Safe Medication Practices found that clear separation cuts wrong-medication errors by 63%. Label each container with the person’s full name. If you’re using a lockbox, put a small sticky note on the front: “John’s Meds,” “Sarah’s Meds.”
Group by type too: oral meds together, patches in a sealed bag, inhalers in their own box, eye drops separate. Keep injectables like insulin in a dedicated spot. Don’t store them next to food-even in the fridge. A Canadian study showed that keeping meds away from food and lab samples reduced cross-contamination by 85%.
Track Expiration Dates Like a Pro
You think your medicine is fine if it’s not moldy. But potency fades long before that. The FDA says 82% of pills still work a year past expiration-if stored right. But at two years? That drops to 65%. At three? Just 42%. And you won’t know unless you check.
Every six months, do a full inventory. Take everything out. Look at the labels. Write the expiration date on a sticky note and stick it to the bottle. Check for color changes, weird smells, or pills that crumble. If it looks off, toss it. Don’t wait for the date. A 2021 FDA study found 27% of degraded meds showed visible color shifts, and 34% had texture changes long before expiration.
For multi-dose items like insulin vials or eye drops, mark the date you opened them. Most lose effectiveness after 28 days, even if the bottle says “use by 2027.” Write “Opened: 1/15/2026” right on the label. This cuts waste and keeps you safe.
Special Cases: Insulin, Inhalers, and More
Insulin needs special attention. Unopened? Always refrigerated between 36-46°F. Once opened? It can stay at room temperature for 14 to 56 days, depending on the type. But don’t leave it on the counter. Put it in a small container inside a drawer. A 2022 American Diabetes Association study found 38% of users store in-use insulin wrong-cutting its effectiveness by up to 30%.
Inhalers? Store them in a plastic box or bag. Accidental presses from being jostled in a drawer can empty them. That’s not just wasteful-it’s dangerous if you need it during an attack. Keep them in a consistent spot, not tucked under towels.
Topical creams, ointments, and even insect repellents? They’re still medications under the law. North Carolina’s Kaitlyn’s Law requires all of them to be stored in original containers with pharmacy labels. Why? Because a child might mistake a steroid cream for hand lotion. There were 127 reported cases between 2018 and 2020 where topical meds were accidentally swallowed.
Build Your Checklist Routine
A checklist only works if you use it. Make it part of your life.
- Monthly: Do a quick visual check. Look for changes in color, texture, or smell. Check if anything’s missing.
- Every 3 months: Review all labels. Are names clear? Are dates visible? Update any that faded.
- Every 6 months: Full inventory. Take everything out. Discard expired or damaged meds. Reorganize. Do this during daylight saving time changes-it’s easy to remember.
- Daily: If you store meds in the fridge, check the temperature once a day. Use a small thermometer. It should stay between 36-46°F. Log it if you can. A 2021 Johns Hopkins study found that people who tracked fridge temps had 98% medication stability versus 76% without.
Keep your checklist printed and taped to the inside of the storage cabinet door. Make it simple: “Check dates? ✅” “Lock closed? ✅” “No new meds added? ✅”

Dispose of Old Meds the Right Way
Never flush pills. Never throw them in the trash unprepared. The EPA says 60-80% of pharmaceuticals end up in waterways when flushed. That’s not just an environmental issue-it’s a public health risk. The U.S. Geological Survey found pharmaceutical residues in 80% of U.S. streams.
Use a drug take-back program. The DEA runs National Prescription Drug Take Back Days twice a year-in April and October. Pharmacies, police stations, and hospitals often have permanent drop boxes. Find one near you. It’s free and safe.
If no drop-off is available, mix pills with something unappetizing: coffee grounds, kitty litter, or dirt. Use a 1:3 ratio-three parts dirt to one part pills. Put it in a sealed container, then toss it. This cuts accidental ingestion by 76%, according to the FDA. Remove labels from bottles before recycling them.
Why This Matters More Than You Think
This isn’t just about keeping kids safe. It’s about making sure your meds actually work when you need them. It’s about preventing a senior from grabbing the wrong bottle because they look alike. It’s about stopping a teen from taking a painkiller because it’s “just lying there.”
A 2023 Consumer Reports survey of 2,500 households found that families using a detailed storage checklist had 89% fewer medication-related incidents-accidental ingestions, wrong doses, expired pills, you name it. That’s not a small win. That’s life-changing.
You don’t need fancy tools. You don’t need to spend hundreds. You just need to be intentional. A checklist isn’t bureaucracy-it’s insurance. For your family. For your health. For your peace of mind.
Can I store all my medications in one box?
No. Storing all medications together increases the risk of mix-ups, especially if multiple people live in the home. Each person’s meds should be separated-ideally in different containers or clearly labeled sections. Mixing types like insulin, inhalers, and topical creams also risks contamination or accidental misuse.
How often should I check expiration dates?
Check every six months. That’s when most households fall behind. Pair it with daylight saving time changes-it’s an easy reminder. Don’t wait for the date to pass. If a pill looks discolored, smells odd, or feels brittle, throw it out immediately.
Is it safe to keep medications in the fridge?
Only if they require it-like insulin or certain antibiotics. Store them away from food and never in the door, where temperatures swing. Use a small, labeled container. Check the fridge temperature daily with a thermometer to keep it between 36-46°F.
What should I do with old or unused medications?
Use a drug take-back program if available. Pharmacies, hospitals, and police stations often have drop boxes. If none exist, mix pills with coffee grounds or kitty litter in a sealed container and throw them in the trash. Never flush them-this pollutes water systems and can harm wildlife and drinking water.
Do I need to keep medications in their original bottles?
Yes. Original bottles have the pharmacy label with the patient’s name, drug name, dosage, and expiration date. Removing them increases the risk of misuse, especially for seniors or children. Even OTC meds like ibuprofen or allergy pills should stay in their original containers.
Next Steps: Start Today
Grab a lockbox. Clear off your bathroom cabinet. Pull out every pill, patch, and spray you have. Check dates. Separate names. Label everything. Lock it up. Write down your next check-in date. Do it now-before someone gets hurt.




Comments (10)
Roisin Kelly
Yeah right, like anyone actually follows this. My mom keeps her meds in the bathroom because it’s ‘convenient.’ She’s 72 and forgets which pill is which every other day. And don’t even get me started on the ‘lockbox’-my cousin’s kid opened hers with a butter knife and ate 12 Advil. Kids are sneaky. This whole checklist is just feel-good nonsense for people who think safety is a Pinterest board.
lokesh prasanth
storage = control. control = fear. fear = power. you think locking pills stops chaos? no. chaos is in the mind. the body knows what it needs. let the child eat the pill. let the system break. then we learn. or dont. either way, life continues.
Malvina Tomja
Let me just say-this is the most irresponsible piece of ‘safety advice’ I’ve seen in years. You’re telling people to lock up their meds like they’re contraband? What’s next, putting a padlock on the aspirin? The FDA says 82% of expired meds still work. So why are we treating our own families like potential criminals? This isn’t safety-it’s medical paranoia dressed up as responsibility.
Barbara Mahone
I appreciate the thoroughness, but I wonder if the tone unintentionally stigmatizes people who need medication. My grandmother takes eight different pills. She doesn’t need a lockbox-she needs someone to help her organize them. The real issue isn’t storage-it’s access to support. Not everyone has the luxury of a ‘dedicated cabinet’ or time to do biweekly inventories. Maybe the checklist should start with: ‘Do you have help?’
Ashok Sakra
my sister took my dad’s heart pill by accident and he died. i was 14. now i keep all meds in a safe in the basement. locked. coded. under a false floor. i even put a camera on it. you think this is overkill? wait until you lose someone. then come back and tell me how chill you are.
Samuel Mendoza
90% reduction? Where’s the study? Oh right-this post cites a ‘Consumer Reports survey’ with no link. Classic. Also, you say ‘never flush’ but the EPA says it’s fine for certain meds. You’re cherry-picking data to scare people. This isn’t safety-it’s clickbait with a side of guilt.
Glenda Marínez Granados
So we’re locking up our meds like they’re nuclear codes… while our kids are scrolling TikTok for 12 hours straight? 😅 At least the pills aren’t addictive. Wait… some are. 🤔
shubham rathee
the bathroom cabinet thing is real i used to keep my antidepressants there and they turned into mush by june. now theyre in a drawer with a rubber band around them. no lockbox needed. just dont be dumb. also why do you need to label every bottle with full names? its not a prison. people know their own meds.
Dee Monroe
I just want to say how deeply moved I am by this. Not because it’s perfect-no checklist ever is-but because it reminds us that love isn’t just in the big moments. It’s in the quiet, daily acts: checking the fridge temperature, writing ‘Opened: 1/15/2026’ on a bottle, taking a second to separate your pills from your husband’s. It’s not about control. It’s about showing up-for your kids, your aging parents, your future self when your hands shake and your memory fades. This isn’t just a guide. It’s a quiet prayer written in sticky notes and lockboxes. Thank you for caring enough to write it.
Rod Wheatley
YES. YES. YES. This is exactly what we need. I’m a nurse, and I’ve seen too many ER visits because someone grabbed the wrong bottle, or the insulin got warm, or the inhaler was empty because it got pressed in a drawer. This checklist? It’s not extra-it’s essential. I print this out and give it to every patient I can. Lockboxes cost $12. A full inventory takes 20 minutes. A life? Priceless. Do it now. Don’t wait for the ‘what if.’ Your future self will thank you. And if you’re reading this and thinking ‘I don’t have time’-you’re already too late. Start today. Right now. Go. I’ll wait.