
For millions of Americans, statin medications are a daily part of life - just like brushing your teeth or taking a multivitamin. But while these drugs have saved countless hearts, they’ve also left a trail of confused, frustrated patients wondering: is the muscle pain worth it?
How Statins Actually Lower Cholesterol
Statins don’t just reduce cholesterol - they reprogram how your liver handles it. These drugs block HMG-CoA reductase, the enzyme your liver uses to make cholesterol. When that enzyme slows down, your liver senses a shortage and pulls more LDL (bad cholesterol) out of your bloodstream to make up the difference. The result? LDL levels drop by 30% to 60%, depending on the statin and dose.
This isn’t just theory. Landmark studies like the 4S trial and the Heart Protection Study showed that people taking statins had about 30% fewer heart attacks and strokes over five years. For someone with a history of heart disease, that’s not a small win - it’s life-changing. Even people without prior heart problems but with high risk (like those with diabetes or very high LDL) see clear benefits.
What’s often overlooked is that statins do more than lower LDL. They calm inflammation in artery walls, stabilize plaque so it’s less likely to rupture, and improve how blood vessels relax and respond to stress. These effects start within weeks - sometimes before LDL even drops significantly. That’s why even people with only mildly elevated cholesterol can benefit if their overall risk is high.
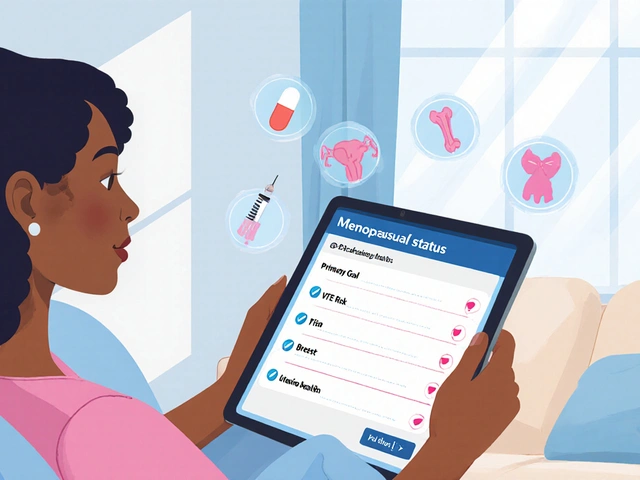
Who Benefits Most From Statins?
Not everyone needs a statin. The guidelines are clear: if you’ve had a heart attack, stroke, or bypass surgery, you’re a strong candidate. Same if you have diabetes and are over 40, or if your LDL is above 190 mg/dL. But for people with moderate risk - say, a 10-year risk of 7.5% to 20% - the decision gets trickier.
Here’s the math: for every 1 mmol/L (39 mg/dL) drop in LDL, your risk of a major heart event falls by about 22%. That means if your LDL is 160 and you drop it to 100, you’re cutting your risk by nearly half. But if your LDL is only 130 and your overall risk is low, the benefit is smaller - maybe a 1 in 100 chance of preventing a heart attack over five years.
Doctors use tools like the ASCVD Risk Calculator to estimate this. But numbers alone don’t tell the whole story. If you’re 55, sedentary, and stressed, and your cholesterol is borderline, lifestyle changes might be enough. If you’re 65, have high blood pressure, smoke, and your LDL is 170 - statins are likely the smarter move.
The Muscle Pain Problem
Let’s talk about the elephant in the room: muscle pain. About 1 in 10 people on statins report aches, cramps, or weakness - usually in the shoulders, thighs, or calves. It’s not always dramatic. Some notice they can’t climb stairs like they used to. Others wake up stiff, like they’ve run a marathon without moving.
Here’s the catch: most of this pain isn’t dangerous. It’s called myalgia - muscle discomfort without actual damage. True muscle breakdown (rhabdomyolysis) is extremely rare - fewer than 1 in 1,000 people per year. But the discomfort is real, and it’s common enough that nearly half of people stop taking statins within a year, according to JAMA Internal Medicine.
Why does this happen? Statins interfere with the production of coenzyme Q10, which helps muscles generate energy. They also affect proteins involved in muscle cell repair. For some, this leads to fatigue and soreness. For others, nothing. Genetics play a role - a variant in the SLCO1B1 gene makes simvastatin more likely to cause muscle issues. But most people don’t get tested for it.

What to Do If You Have Muscle Pain
If you start feeling sore after beginning a statin, don’t quit cold turkey. Talk to your doctor first. Here’s what usually works:
- Switch statins. Not all statins are the same. Pravastatin and fluvastatin are less likely to cause muscle pain than simvastatin or atorvastatin. Many patients find relief just by changing brands.
- Lower the dose. Sometimes half a pill works just as well for cholesterol control - and causes far fewer side effects.
- Try every other day. Some people can take rosuvastatin or atorvastatin every other day and still keep LDL low. This isn’t for everyone, but it’s worth exploring.
- Check your vitamin D and thyroid levels. Low vitamin D or underactive thyroid can make muscle pain worse - and mimic statin side effects.
- Consider CoQ10 supplements. Some studies show CoQ10 helps reduce muscle discomfort, though results aren’t consistent. It’s low-risk and cheap - often worth a 3-month trial.
Don’t ignore severe pain, dark urine, or extreme weakness. Those could be signs of rhabdomyolysis. Get your creatine kinase (CK) levels checked immediately.
Real Stories, Real Choices
One patient I know - let’s call her Maria - started on simvastatin after a mild heart attack. Within three months, she couldn’t walk her dog without stopping to rest. Her legs felt heavy, like they were filled with cement. She thought it was aging. Her doctor suggested switching to pravastatin. Within two weeks, she was walking again. Her LDL stayed at 85.
Another man, 68, took atorvastatin for five years. He felt fine - until he started doing yoga. His shoulders and hips ached constantly. He stopped the pill on his own. His LDL jumped to 190. He went back on, but at half the dose. The pain returned. He switched to rosuvastatin 10 mg every other day. His cholesterol stayed under 100. The pain vanished.
These aren’t outliers. They’re common. Statins aren’t one-size-fits-all. What works for your neighbor might wreck your quality of life.
Cost, Compliance, and Long-Term Thinking
Atorvastatin and rosuvastatin are now generic. You can get a 30-day supply for under $5 at Walmart or through GoodRx. That’s less than a coffee a week. But if you’re in pain, no price makes it worth it.
Adherence is the biggest problem. Studies show that people who stop statins within a year have a 30% higher risk of heart attack. But if you’re suffering, the answer isn’t to push through - it’s to find a version that works for you.
Many patients think: “I’ll take it for a few months, then stop.” But statins work best when taken daily, long-term. The benefits build slowly. The cardiovascular protection isn’t immediate - it’s cumulative. Missing doses or stopping and starting undermines the entire purpose.
The Bottom Line
Statins are one of the most effective drugs ever developed for preventing heart disease. For the right person, they’re a game-changer. But they’re not magic pills. They’re tools - and like any tool, they need to fit the user.
If you’re on a statin and feel fine - keep taking it. Your heart will thank you.
If you’re on a statin and feel awful - don’t assume it’s normal. Don’t assume you’re just getting older. Talk to your doctor. Try a different statin. Adjust the dose. Test your CoQ10, vitamin D, and thyroid. There’s almost always a better fit.
And if you’re unsure whether you need one at all - ask for your 10-year risk score. Don’t just take a pill because your doctor said so. Understand why. Weigh the numbers. Consider your lifestyle. Then decide.
Statin therapy isn’t about fear. It’s about control. And control means knowing when to use it - and when to find another way.
Do statins really prevent heart attacks?
Yes - and the evidence is strong. In people with known heart disease, statins reduce the risk of another heart attack or stroke by about 30% over five years. For those at high risk but without prior events, the reduction is still significant - around 20-25%. The benefit is greatest in people with higher baseline LDL or other risk factors like diabetes or high blood pressure. Studies like the 4S trial and Heart Protection Study followed tens of thousands of patients and confirmed these results.
How common is muscle pain with statins?
Muscle pain (myalgia) occurs in about 5% to 10% of people taking statins. Some studies report higher numbers - up to 29% - especially when patients are actively asked about symptoms. The pain is usually mild to moderate and affects the legs, shoulders, or lower back. True muscle damage (rhabdomyolysis) is rare - fewer than 0.1% of users. Many people mistake normal aging or exercise soreness for statin side effects, which is why reports vary.
Can I stop statins if I have muscle pain?
Don’t stop without talking to your doctor. Stopping statins suddenly increases your risk of heart attack or stroke, especially if you’ve had prior cardiovascular issues. Instead, ask about switching to a different statin (like pravastatin or fluvastatin), lowering the dose, or trying an every-other-day schedule. Blood tests for creatine kinase (CK) can rule out serious muscle damage. Many people find relief by adjusting the medication - not by quitting entirely.
Are there alternatives to statins for lowering cholesterol?
Yes, but none match statins’ proven ability to prevent heart attacks. Ezetimibe lowers LDL by about 15-20% and is often added to statins. PCSK9 inhibitors (like evolocumab) can cut LDL by 60% but require injections and cost thousands per year. Bempedoic acid is a newer oral option for those who can’t tolerate statins. Lifestyle changes - diet, exercise, weight loss - help, but rarely lower LDL enough on their own for high-risk patients. Statins remain the gold standard for risk reduction.
Do I need to take statins for life?
For most people who start statins for high risk or existing heart disease, yes - long-term use is recommended. The benefits are cumulative, and stopping increases risk within months. However, if you’re on a statin for borderline risk and you make major lifestyle changes - like losing 30 pounds, quitting smoking, and exercising regularly - your doctor might reevaluate after a year. Some patients with very low risk after lifestyle improvements can safely stop, but this requires careful monitoring and repeated risk assessments.
Can CoQ10 supplements help with statin muscle pain?
Some people report relief from muscle pain after taking CoQ10 supplements, and the theory makes sense - statins lower CoQ10 levels, which muscles need for energy. But clinical trials show mixed results. A few small studies found benefit; larger ones didn’t. Still, CoQ10 is safe and inexpensive (typically $10-$15 per month). If you’re having muscle discomfort, trying 100-200 mg daily for 6-8 weeks is a reasonable, low-risk option to discuss with your doctor.
What Comes Next?
If you’re on a statin and feeling fine - keep going. Don’t let fear of side effects override the proven benefits.
If you’re struggling with pain - don’t suffer in silence. Ask your doctor about alternatives. You might be one switch away from feeling like yourself again.
And if you’re not sure you need one - get your risk calculated. Ask about your LDL, your blood pressure, your family history. Make the decision with your doctor, not from a Reddit post or a TV commercial.
Heart disease doesn’t announce itself. But statins, when used right, can keep it at bay - without wrecking your legs in the process.



Comments (8)
Bailey Sheppard
Statins saved my dad’s life after his bypass. He was skeptical about the muscle pain too, but switched to pravastatin and now hikes every weekend. It’s not magic, but it’s one of the few things that actually works when you’ve got the numbers stacked against you.
Girish Pai
Let’s be clear - statins are the only evidence-based intervention that directly modulates LDL-C via HMG-CoA reductase inhibition, reducing ASCVD events by 22% per mmol/L reduction. The so-called 'muscle pain' is often psychosomatic or confounded by vitamin D deficiency. In India, we don’t have the luxury of overthinking this - we take the pill or die young.
Kristi Joy
If you’re experiencing muscle discomfort, please don’t just quit. I’ve seen too many people give up because they think it’s 'just aging.' Talk to your doctor - try a different statin, check your vitamin D, maybe even try CoQ10 for a couple months. You deserve to feel good while staying healthy. It’s not weakness to ask for a better fit - it’s wisdom.
Hal Nicholas
Everyone’s jumping on the statin bandwagon like it’s the new Jesus. Meanwhile, Big Pharma’s been quietly funding every 'study' that says it’s safe. My neighbor took it for six months and ended up in the ER with rhabdo. They told him it was 'rare.' Rare doesn’t mean impossible - and it doesn’t mean it’s worth it for someone with borderline numbers.
Louie Amour
You people are ridiculous. If you can’t handle a $5 pill that prevents heart attacks, maybe you shouldn’t be allowed to drive. Your 'muscle pain' is just laziness dressed up as a medical condition. I’ve been on atorvastatin for 12 years, never felt a thing, and I work two jobs. Stop making excuses and take your medicine.
Kristina Williams
Statins are a government plot to make us dependent on pills. They lower CoQ10 on purpose so you need supplements - and then they sell you the supplements too. I read a blog that said the FDA knew about the muscle damage since the 90s but buried it. Your doctor won’t tell you this, but the truth is out there.
Shilpi Tiwari
The SLCO1B1 polymorphism is critical here - especially in South Asian populations where the C allele frequency is higher, increasing statin myopathy risk. Pravastatin and fluvastatin have lower hepatic uptake, making them preferable in genetically susceptible individuals. Also, check your 25(OH)D levels - deficiency exacerbates myalgia synergistically. This isn’t anecdotal - it’s pharmacogenomics.
Christine Eslinger
There’s a quiet truth here: statins aren’t about fear. They’re about giving people back control - control over their future, not just their cholesterol numbers. The pain some feel isn’t weakness, it’s biology. And the fact that we can adjust the dose, switch the drug, or add CoQ10 means medicine isn’t one-size-fits-all - it’s personalized. That’s the real win. Don’t quit because it hurts. Don’t stay because you’re scared. Find the version that lets you live - not just survive.