
When someone has symptoms of more than one autoimmune disease at the same time-like joint pain from rheumatoid arthritis, skin tightening from scleroderma, and lung trouble from interstitial disease-it’s not always easy to put a name to it. These aren’t just random combinations. They’re autoimmune overlap syndromes, real medical conditions where the immune system attacks multiple tissues at once, blurring the lines between classic diseases. Unlike single autoimmune disorders, overlap syndromes don’t fit neatly into textbooks. They’re messy, complex, and often missed-leading to years of confusion for patients and doctors alike.
What Exactly Is an Autoimmune Overlap Syndrome?
An autoimmune overlap syndrome happens when a person meets the diagnostic criteria for two or more distinct connective tissue diseases (CTDs). The five main ones involved are systemic lupus erythematosus (SLE), scleroderma, polymyositis, rheumatoid arthritis (RA), and Sjögren’s syndrome. But here’s the catch: there’s no official checklist for overlap syndromes. The American College of Rheumatology and European League Against Rheumatism have clear rules for each individual disease, but not for when they mix together. That’s why many patients get stuck in a diagnostic gray zone called undifferentiated connective tissue disease (UCTD) for years before their true pattern emerges.
Some overlap syndromes are well-defined by their unique antibody signatures. For example, mixed connective tissue disease (MCTD) is almost always tied to high levels of anti-U1-RNP antibodies-often above 1:10,000. Patients with MCTD typically have puffy hands, Raynaud’s phenomenon (fingers turning white in the cold), swollen joints, and sometimes lung or muscle involvement. Another common type is antisynthetase syndrome, which shows up with anti-Jo-1 antibodies in about 80% of cases. These patients often struggle with muscle weakness, scaly hands (called mechanic’s hands), and serious lung inflammation. Then there’s PM/Scl overlap, where anti-PM/Scl antibodies link muscle inflammation with skin thickening. These aren’t random clusters. Each has a fingerprint in the blood that helps doctors spot them.
Why Diagnosis Takes So Long
It’s not uncommon for patients to wait over 18 months to get a correct overlap diagnosis. That’s six months longer than the average delay for a single autoimmune disease. Why? Because symptoms overlap so much. A patient with joint pain and fatigue might be treated for lupus, while their lung scarring goes unnoticed. Another might be labeled as having myositis, but their dry eyes and mouth-classic Sjögren’s signs-are dismissed as unrelated. Doctors often look for one clear disease, not multiple. And when tests come back inconclusive, the default response is to wait and watch.
One patient on a myositis forum described seeing seven specialists over three years before someone connected her muscle weakness with her tight, shiny skin. "They kept treating me for one thing while ignoring the rest," she wrote. That’s the pattern. Fragmented care. Siloed specialties. No one looking at the whole picture. A 2021 survey from the Myositis Association found that 72% of patients with overlap syndromes experienced delays longer than a year. Many ended up in emergency rooms because their symptoms worsened without coordinated treatment.
Key Autoantibodies and Their Clues
Autoantibodies are the secret decoder ring for overlap syndromes. They’re not just markers-they’re predictors. Here’s what matters most:
- Anti-U1-RNP: The hallmark of MCTD. Present in 83% of cases, with 95% specificity. If you see this antibody with Raynaud’s and puffy fingers, MCTD is likely.
- Anti-Jo-1: The most common in antisynthetase syndrome. Found in 75-80% of cases. Associated with myositis, interstitial lung disease (ILD), and mechanic’s hands.
- Anti-PL-7 and Anti-PL-12: Less common but still important. These are the next most frequent synthetase antibodies after Jo-1.
- Anti-PM/Scl: Seen in 2-5% of scleroderma patients and 8-10% of polymyositis cases. Points to a mix of skin tightening and muscle inflammation.
These antibodies aren’t just diagnostic tools-they guide treatment. For example, if a patient has anti-Jo-1 and early lung involvement, starting immunosuppression sooner can prevent irreversible scarring. Missing the antibody means missing the window to act.
When Three or More Diseases Collide: Multiple Autoimmune Syndrome
Some patients go beyond two overlapping conditions. When three or more autoimmune diseases appear together, it’s called Multiple Autoimmune Syndrome (MAS). This isn’t rare-it’s underrecognized. Type 1 MAS includes myasthenia gravis, thymoma, and polymyositis. Type 2 often involves Sjögren’s, rheumatoid arthritis, and autoimmune thyroid disease. Type 3 is the broadest, covering everything from type 1 diabetes to vitiligo to pernicious anemia.
Patients with MAS are often younger, female, and have a family history of autoimmunity. Their challenge isn’t just managing multiple symptoms-it’s avoiding treatment conflicts. A drug that helps one condition might worsen another. For example, TNF inhibitors used for RA can trigger lupus-like reactions. Steroids might calm inflammation but increase diabetes risk in someone already prone to it. The bigger the list of diagnoses, the harder it is to balance treatment.
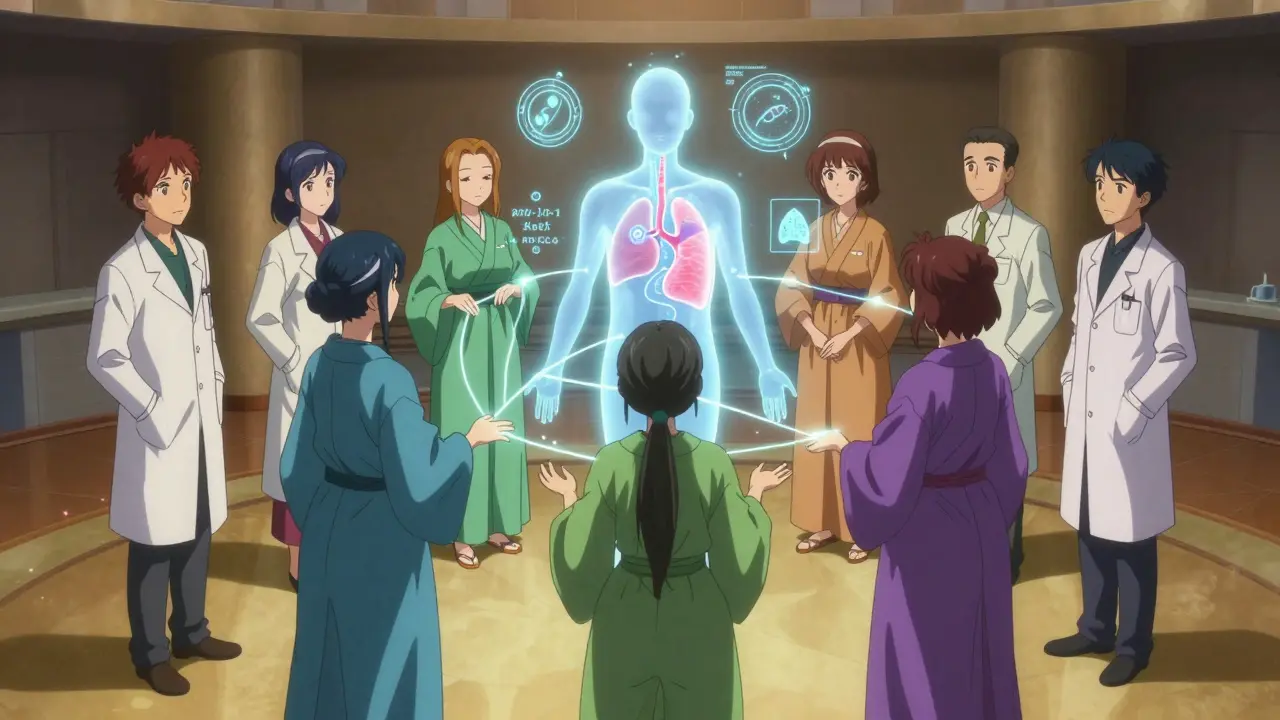
How Care Should Be Coordinated-Not Fragmented
The biggest problem in overlap syndromes isn’t the disease itself-it’s the system. Most patients see a rheumatologist for joints, a pulmonologist for lungs, a dermatologist for skin, and a gastroenterologist for dry mouth. No one connects the dots. That’s why care coordination isn’t optional-it’s lifesaving.
Top centers like Johns Hopkins, Mayo Clinic, and Hospital for Special Surgery now use dedicated care coordinators. These aren’t nurses or administrative staff-they’re specialized clinicians who track all aspects of the patient’s condition. They schedule appointments across specialties, review lab results together, adjust medications based on cross-system effects, and serve as the patient’s single point of contact.
One internal study from the Cleveland Clinic showed that patients with a care coordinator had 35% fewer hospitalizations and 42% better medication adherence. Why? Because someone was watching the whole picture. They caught a drug interaction before it caused liver damage. They noticed rising lung function numbers and adjusted therapy before symptoms worsened. They reminded the patient to get a pneumonia shot because they were on three immunosuppressants.
Treatment: Balancing Act, Not One-Size-Fits-All
There’s no standard treatment for overlap syndromes because no two patients are the same. But there are proven starting points. Most patients begin with low-dose corticosteroids-like prednisone at 0.5 to 1 mg per kilogram of body weight-plus one immunosuppressant. Methotrexate or mycophenolate mofetil are common first choices.
But if lung disease is the main problem, the game changes. For antisynthetase syndrome with interstitial lung disease, rituximab has shown 60-70% success in stabilizing lung function over 12 months. In March 2023, the FDA approved tocilizumab specifically for this use after a phase 3 trial showed a 55% drop in disease progression compared to placebo.
For MCTD with severe arthritis or skin involvement, newer drugs like anifrolumab (currently in phase 2 trials) are being tested. The goal isn’t to cure-it’s to control. The American College of Rheumatology’s 2023 guidelines push for a "treat-to-target" approach: keep lung function above 80% predicted, skin score below 15, and arthritis in minimal disease activity. That’s measurable. That’s actionable.
But overtreating is just as dangerous. A 2019 study found that 35% of overlap patients were on three or more immunosuppressants-despite little evidence that stacking them helps. More drugs mean more infections. One study showed 28% of patients on triple therapy got serious infections, compared to 15% on dual therapy. Sometimes, less is more.

The Future: AI, Biomarkers, and Personalized Care
The field is moving fast. In January 2023, the NIH launched a $15 million project to find biomarkers that predict who will develop overlap syndromes and how they’ll respond to treatment. Meanwhile, AI is stepping in. A 2022 study in Nature Medicine used machine learning to analyze electronic health records and predict overlap syndrome development with 82% accuracy-up to a year before symptoms became obvious.
Specialized centers are also developing composite disease activity scores that combine muscle strength, lung function, skin thickness, and joint counts into one number. Think of it like a dashboard for autoimmune health. Instead of tracking five different metrics, doctors get one clear signal: Is the patient improving, stable, or worsening?
Industry analysts predict the market for overlap syndrome treatments will grow 7.2% annually through 2028. Why? Because recognition is rising. More patients are being diagnosed earlier. More drugs are being tested specifically for these complex cases. And more clinics are building teams to handle them.
What Patients Can Do
If you suspect you have an overlap syndrome, here’s what helps:
- Keep a symptom journal. Note when joint pain flares, when your skin tightens, when you get short of breath.
- Ask for autoantibody testing. Don’t assume your rheumatologist will order it. Request anti-U1-RNP, anti-Jo-1, anti-PM/Scl, and others if your symptoms don’t fit one disease.
- Push for a pulmonary function test and high-resolution CT scan. Interstitial lung disease is common and often silent until it’s advanced.
- Seek out a center with a dedicated overlap or multidisciplinary autoimmune clinic. These aren’t just big hospitals-they’re teams built for complexity.
- Ask for a care coordinator. If your clinic doesn’t have one, request it. Your health depends on coordination, not just expertise.
Autoimmune overlap syndromes aren’t a dead end. They’re a call for better care. The science is catching up. The treatments are improving. But without coordinated, patient-centered care, even the best drugs won’t help.
Can you have an autoimmune overlap syndrome without meeting full criteria for either disease?
Yes. Many patients have what’s called undifferentiated connective tissue disease (UCTD), where symptoms point to more than one autoimmune condition but don’t fully meet classification criteria. About 30-40% of these patients eventually develop a defined overlap syndrome within five years. The presence of specific autoantibodies, like anti-U1-RNP or anti-Jo-1, often signals that a full overlap is coming-even if symptoms are still mild.
Are overlap syndromes hereditary?
They’re not directly inherited like a genetic disorder, but having a family history of autoimmunity increases risk. If close relatives have lupus, rheumatoid arthritis, Sjögren’s, or thyroid disease, your chance of developing an overlap syndrome is higher. It’s not about one gene-it’s about a predisposition where the immune system is more likely to go off track.
Can stress trigger or worsen an overlap syndrome?
Stress doesn’t cause autoimmune diseases, but it can trigger flares. Chronic stress raises cortisol and inflammatory markers, which can push an already unstable immune system into overdrive. Many patients report symptom worsening after major life events-loss, surgery, or prolonged emotional strain. Managing stress through sleep, mindfulness, or therapy isn’t optional-it’s part of treatment.
Is it safe to take multiple immunosuppressants for overlap syndromes?
It can be, but only under close supervision. Combining drugs like methotrexate, mycophenolate, and steroids increases infection risk-from pneumonia to sepsis. Studies show 28% of patients on three or more immunosuppressants get serious infections, compared to 15% on two. The goal is to use the fewest drugs possible to control symptoms. Sometimes, switching to a single targeted therapy like rituximab or tocilizumab is safer and more effective than stacking older drugs.
Why isn’t there a single test to diagnose overlap syndromes?
Because overlap syndromes aren’t one disease-they’re patterns of multiple diseases. No single blood test or scan can capture that complexity. Diagnosis requires combining clinical symptoms, antibody results, imaging (like lung CTs), and sometimes muscle or skin biopsies. It’s a puzzle. The right antibodies help, but you still need the full picture: what you feel, what doctors see, and what tests show.
What’s the difference between MCTD and lupus?
MCTD and lupus share symptoms like joint pain and fatigue, but MCTD is defined by high-titer anti-U1-RNP antibodies and the absence of severe kidney or brain involvement-common in lupus. MCTD patients often have puffy hands and Raynaud’s more intensely than lupus patients. Lung disease and muscle weakness are also more prominent in MCTD. Treatment is similar, but MCTD rarely needs aggressive kidney-targeted therapy, which lupus sometimes does.
Next Steps: What to Do If You’re Diagnosed
If you’ve been told you have an overlap syndrome, start by asking three questions: What’s my main antibody? What’s my most serious organ involvement? And who’s coordinating my care? Write down your symptoms, your medications, and your specialist appointments. Bring them to your next visit. Don’t wait for the system to fix itself. The most effective treatment isn’t always the newest drug-it’s the person who’s paying attention to all of you, not just one part.



Comments (10)
Donny Airlangga
This post hit hard. I’ve been stuck in UCTD limbo for four years. Every specialist saw one piece-joints, lungs, dry eyes-but no one connected them until I walked into a rheumatology clinic that actually had a coordinator. That person saved my life.
Evan Smith
So let me get this straight-we’ve got AI predicting autoimmune overlaps before symptoms show up, but most docs still treat them like they’re five separate patients in one body? That’s not medicine, that’s a buffet of neglect.
christy lianto
I’m a nurse who works in rheum. I’ve seen the same thing over and over: patients get passed around like a hot potato. One day it’s ‘probably lupus,’ next week ‘maybe scleroderma,’ then ‘oh wait, your lungs are failing.’ No one’s watching the whole board. The care coordinators? They’re the unsung heroes. Push for one. They exist.
Manish Kumar
You know, in ancient India, they believed the body was a temple of five elements-earth, water, fire, air, ether. When one element is out of balance, the whole temple trembles. Modern medicine splits the temple into rooms and sends each room to a different priest. But the soul-the immune system-doesn’t care about departments. It just screams. And we keep calling it ‘undiagnosed.’ Maybe we’re not failing the science-we’re failing the soul.
Molly Silvernale
Anti-U1-RNP? Anti-Jo-1? These aren’t just letters and numbers-they’re whispered secrets in our blood. The immune system isn’t confused-it’s trying to tell us something. And we’re too busy labeling the symptoms to hear the scream behind them. We need to stop treating diseases like Lego sets and start listening to the whole damn structure.
Dave Old-Wolf
My mom had MCTD. They gave her steroids for years, then switched to mycophenolate. Her lung function dropped anyway. Then they tried rituximab-and boom, stopped the decline. I wish someone had told us about that antibody test sooner. Don’t wait. Ask for it.
swati Thounaojam
they never tested me for jo-1 until i begged. by then my lungs were already scarred. dont wait. ask for the test.
Annette Robinson
Just want to say-this isn’t just about medicine. It’s about being seen. I spent years feeling like my pain was ‘in my head’ because no one could fit me into a box. Finding out I had antisynthetase syndrome didn’t cure me-but it finally made me feel real. If you’re reading this and you feel lost-you’re not alone. Keep pushing. Your body deserves to be heard.
Ken Porter
7.2% market growth? So now it’s a profit center? Cool. Meanwhile, patients are still getting passed between specialists like a broken phone. Someone needs to fix the system before Big Pharma turns this into a subscription model.
Prakash Sharma
Who the hell wrote this? Some American doctor with a grant? In India, we don’t have access to rituximab or care coordinators. We have one rheumatologist for 5 million people. You talk about biomarkers and AI like it’s a luxury. For us, it’s a fantasy. This post is beautiful-but it’s written for the 1%. The rest of us are just trying to survive.