When you pick up a prescription, you might see two options: the brand-name pill you’ve always taken, or a cheaper generic version. You might wonder-does the generic really work the same? The answer lies in two technical terms: bioavailability and bioequivalence. These aren’t just jargon. They’re the scientific backbone that lets pharmacists, doctors, and regulators say with confidence that a $5 generic is just as safe and effective as a $50 brand-name drug.
What Bioavailability Really Means
Bioavailability answers one simple question: How much of the drug actually gets into your bloodstream?
Imagine you swallow a pill. It travels through your stomach, gets absorbed in your intestines, and then heads to your liver. Along the way, some of it breaks down. Some doesn’t get absorbed at all. What’s left that makes it into your blood? That’s bioavailability.
It’s measured using two key numbers: AUC (area under the curve) and Cmax (maximum concentration). AUC tells you the total amount of drug your body is exposed to over time. Cmax tells you how high the drug spikes in your blood after you take it. These numbers come from drawing blood samples at timed intervals after dosing-usually in healthy volunteers.
There are two types of bioavailability:
- Absolute bioavailability: Compares the drug’s absorption when taken orally versus directly into the bloodstream via IV. IV is always 100% bioavailable-no digestion, no liver breakdown. If an oral pill gives you 60% of the IV dose, its absolute bioavailability is 60%.
- Relative bioavailability: Compares two different versions of the same drug, like a brand pill versus a generic. This is the foundation for bioequivalence testing.
For example, a drug might have 50% absolute bioavailability because only 70% of the dose gets absorbed in the gut, and then 30% gets broken down by the liver before it ever reaches circulation. That’s normal. It doesn’t mean the drug is weak-it just means your body handles it a certain way.
What Bioequivalence Is-and Why It Matters
Bioequivalence doesn’t look at one drug. It compares two. Specifically, it asks: Does the generic version deliver the same amount of active ingredient, at the same speed, as the brand-name version?
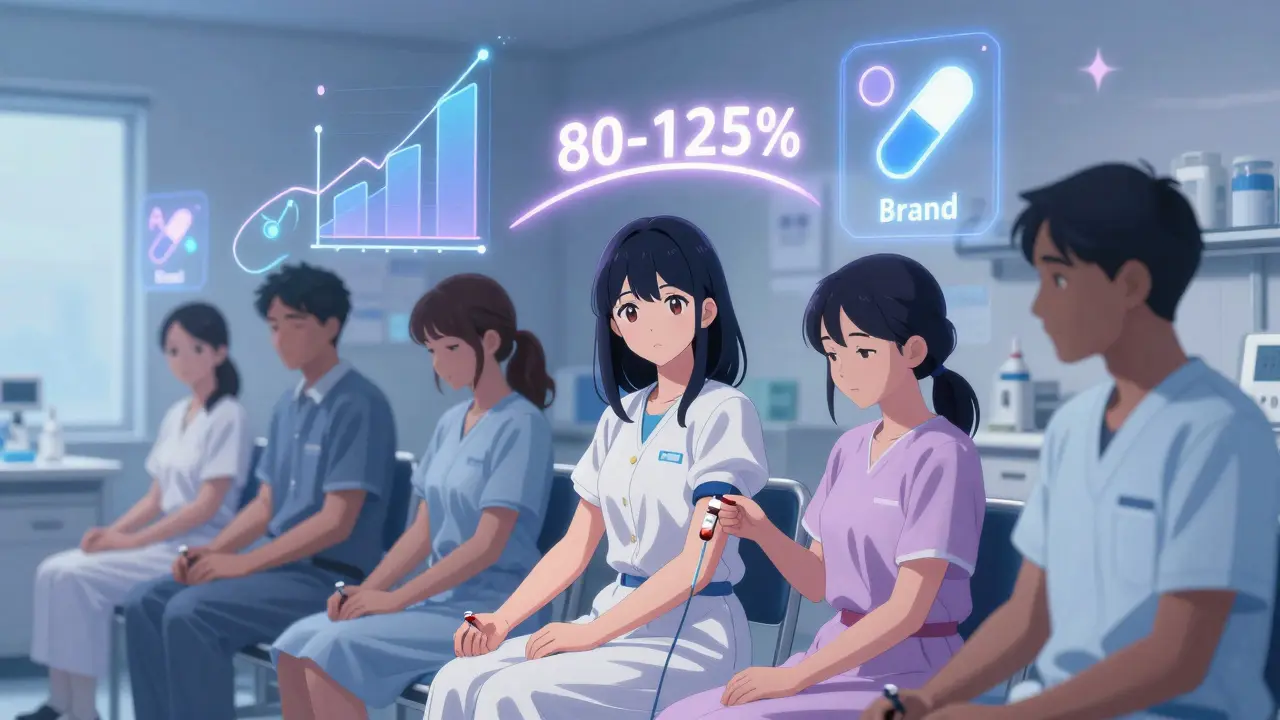
The FDA and other global regulators don’t just assume they’re the same. They require proof. That proof comes from a head-to-head study. Healthy volunteers take both the brand drug and the generic, each in a separate period, with a washout period in between. Blood samples are taken over 72 hours. AUC and Cmax are calculated for each.
Here’s the rule: the 90% confidence interval for the ratio of the generic’s AUC and Cmax to the brand’s must fall between 80% and 125%. This is called the 80/125 rule.
Let’s say the brand’s average AUC is 100 units. For the generic to be bioequivalent, its average AUC must be between 80 and 125 units. That’s a 20% range on either side. Why not 100% exactly? Because no two pills are identical. Manufacturing has tiny variations. The body absorbs drugs with natural variability. The 80/125 rule accounts for that.
It’s not about being identical. It’s about being therapeutically equivalent. If both drugs hit the same blood levels within this range, they’re expected to work the same way in your body.
Key Differences Between Bioavailability and Bioequivalence
It’s easy to mix them up. Here’s how they’re different:
| Aspect | Bioavailability | Bioequivalence |
|---|---|---|
| Definition | How much of a single drug formulation enters the bloodstream | Comparison of two drug products to see if they deliver the same exposure |
| Scope | Single product | Two products (test vs. reference) |
| Goal | Understand absorption profile | Prove interchangeability for generics |
| Used in | Drug development, formulation design | Generic drug approval |
| Statistical requirement | None | 90% CI must be 80-125% |
Bioavailability is like measuring how fast a car goes from 0 to 60. Bioequivalence is like comparing two different models of the same car to see if they accelerate the same way. One tells you about the car. The other tells you if the two cars are interchangeable.
Why the 80/125 Rule Works
Some people think the 80/125 rule is too loose. What if a generic delivers 79%? Would it fail? What if it delivers 126%? Would it be dangerous?
The answer is in the statistics. The rule uses a 90% confidence interval, not just a point estimate. That means regulators are 90% sure the true difference between the two drugs falls within that 80-125% range. It’s not about the average-it’s about the range of likely values.
Also, pharmacokinetic data doesn’t follow a straight line. It’s multiplicative. That’s why they use log-transformation. A 20% increase isn’t just +20-it’s multiplied by 1.2. The 80/125 rule was chosen because decades of real-world data show that within this range, therapeutic outcomes are essentially identical.
Dr. Robert Lionberger of the FDA put it plainly: “The 80/125 rule balances patient safety with access to affordable medicine.” And the data backs it up. Between 2010 and 2020, 99.7% of approved generics met this standard. And in real-world use, studies show that over 97% of patients experience no difference when switching.
When the Rule Isn’t Enough
Not all drugs are created equal. Some have a narrow therapeutic index-meaning the difference between an effective dose and a toxic one is tiny. Warfarin, lithium, levothyroxine, and some anti-seizure drugs fall into this category.
For these, the standard 80/125 rule isn’t tight enough. The FDA has set stricter limits for some of them. For warfarin, the AUC range is narrowed to 90-112%. Cmax stays at 80-125%, because peak levels matter less than total exposure for this drug.
And that’s where controversy pops up. Some pharmacists report patients switching from brand to generic levothyroxine experiencing subtle changes in thyroid levels-even when the generic passed bioequivalence testing. One Reddit user noted multiple patients complaining of fatigue or palpitations after switching. Is this bioequivalence failing? Or is it something else?
Experts like Dr. Lawrence Lesko argue that the one-size-fits-all approach doesn’t work for all drugs. He’s pushed for tailored limits based on drug class. The FDA agrees in practice-just not in policy. They’ve made exceptions for specific drugs, but haven’t changed the general rule.
Studies show that when patients report issues with generics, only about 3-4% of cases are confirmed as true bioequivalence failures. The rest? Often adherence problems, placebo effects, or unrelated health changes.

How These Studies Are Done
Don’t think it’s just a quick lab test. Bioequivalence studies are complex, expensive, and tightly controlled.
Here’s what happens:
- 24 to 36 healthy volunteers are recruited.
- They fast overnight. Food can change how a drug is absorbed-so studies are done under fasting conditions.
- Each volunteer takes the brand drug in one period, then the generic in another, with a 1-2 week washout.
- Blood is drawn 12 to 18 times over 72 hours.
- Samples are analyzed using high-precision mass spectrometry to measure exact drug concentrations.
- Statistical analysis is done on log-transformed AUC and Cmax values.
It takes 3-6 months to design and run one study. And it’s not just the FDA. The European Medicines Agency (EMA), Health Canada, and others have nearly identical requirements. That’s why a generic approved in the U.S. is usually approved in Europe too.
Real-World Impact
In 2022, the FDA approved 752 generic drugs. That’s 91% of all prescriptions filled in the U.S.-but only 22% of total drug spending. Without bioequivalence standards, generics wouldn’t exist. Or they’d be risky.
For patients, this means lower costs. A month’s supply of a brand-name statin might cost $150. The generic? $10. That’s life-changing for people on fixed incomes.
For the system, it means billions saved. The U.S. saved $370 billion in 2022 just from generic drug use, according to the Generic Pharmaceutical Association. That money goes to hospitals, insurers, and patients.
And the science keeps evolving. The FDA is now exploring ways to use physiologically-based pharmacokinetic (PBPK) modeling for complex drugs-like patches, inhalers, or injectables-where traditional blood tests don’t capture what’s happening in the tissue. In the future, we might see more in vitro (lab-based) tests replacing some animal or human studies.
What You Should Know as a Patient
If you’re taking a generic drug and feel fine-stick with it. The odds are overwhelmingly in your favor.
If you switch from brand to generic and notice something off-like new side effects, less energy, or worse symptoms-don’t assume it’s your fault. Talk to your doctor or pharmacist. They can check your blood levels (for drugs like warfarin or thyroid meds) or suggest switching back.
For most drugs, bioequivalence means no difference. For a few, it means you need to be a little more careful. But the system is built to catch those cases.
Bottom line: Bioavailability tells you how a drug works in your body. Bioequivalence tells you that two versions of that drug work the same way. And for the vast majority of medications, that’s enough to trust the cheaper option.
What’s the difference between bioavailability and bioequivalence?
Bioavailability measures how much of a single drug enters your bloodstream. Bioequivalence compares two drugs-usually a generic and brand-to see if they deliver the same amount of drug at the same rate. Bioavailability is about one product. Bioequivalence is about two.
Why does the FDA use the 80/125 rule for bioequivalence?
The 80/125 rule is based on decades of data showing that when two drugs have bioavailability ratios within this range, their clinical effects are essentially identical. It accounts for natural variation in how people absorb drugs and ensures generics are safe and effective without being overly strict. The rule uses a 90% confidence interval on log-transformed data, which better reflects how drug absorption works in the body.
Can a generic drug be less effective than the brand?
Legally approved generics must meet strict bioequivalence standards. In over 99% of cases, they work the same. Rarely, patients report differences with narrow therapeutic index drugs like levothyroxine or warfarin. In those cases, the issue might be due to formulation differences that aren’t fully captured by standard tests. Always report changes to your doctor.
Are bioequivalence studies done on real patients?
No. Bioequivalence studies are done in healthy volunteers under controlled conditions. This is because researchers need to isolate how the drug behaves without interference from disease, other medications, or lifestyle factors. Real-world effectiveness is monitored after approval through pharmacovigilance systems.
Why do some people say generics don’t work for them?
Most of the time, it’s not the drug. People may notice changes due to placebo effects, stress, diet, sleep, or other medications. In rare cases, especially with narrow therapeutic index drugs, small formulation differences can matter. But studies show only about 3-4% of reported issues are medically confirmed as bioequivalence-related. Always consult your doctor before switching back to brand.



Comments (15)
Miriam Piro
Okay but have you ever stopped to think that the FDA is just a puppet of Big Pharma? 🤔 They let generics pass with 80-125% because they don’t want you to know that the fillers in generics are laced with microplastics from the same factories that make your phone chargers. I’ve seen people go from feeling great on brand to depressed, bloated, and dizzy on generic - it’s not placebo, it’s poison. And they call it science? 😒
Olivia Goolsby
Let me tell you something, folks: this whole bioequivalence thing is a scam dressed up in lab coats. The 80/125 rule? That’s not science - that’s corporate math! They’re not testing for therapeutic equivalence - they’re testing for profit equivalence. And don’t get me started on the ‘healthy volunteers’ - who are these people? Are they on SSRIs? Do they have leaky gut? Are they even human? I’ve seen a cousin switch to generic levothyroxine and start having heart palpitations - they told her it was ‘stress’ - LOL. No. It’s the talc. It’s always the talc.
Alex Lopez
Interesting perspective - but let’s not confuse anecdote with data. The FDA’s 99.7% approval rate for generics isn’t magic - it’s rigor. Yes, there are rare exceptions with narrow-therapeutic-index drugs, and yes, formulation differences can matter. But the system is designed to catch those outliers. And for the record: if you’re having side effects after switching, your doctor can check serum levels. It’s not conspiracy - it’s pharmacokinetics. 😊
Satyakki Bhattacharjee
Generic drugs are good for poor people. But rich people want brand because they think it is better. This is not science. This is belief. In India, we use generics every day. No one dies. No one cries. We live. Simple.
Kishor Raibole
Let me be perfectly clear: the pharmaceutical industry does not operate in the interest of the patient - it operates in the interest of the shareholder. The bioequivalence standards are a carefully constructed illusion, designed to pacify the masses while the real profits are made in the margins of inactive ingredients, patent extensions, and regulatory loopholes. The 80/125 rule? It’s a fig leaf. And the fact that we accept it as gospel is a testament to our collective surrender to institutional authority.
Liz MENDOZA
I’ve been a pharmacist for 18 years, and I’ve seen patients switch from brand to generic and back again dozens of times. For 98% of them? Zero difference. But for the 2% who say they feel ‘off’? I listen. I check labs. I don’t dismiss them. I don’t assume it’s in their head. Sometimes it’s the filler. Sometimes it’s anxiety. Sometimes it’s both. But if you’re worried? Talk to your provider. You’re not crazy. And you deserve to feel safe in your meds.
dean du plessis
I’ve been on generics for years. No issues. No drama. Just cheaper pills that do the job. Why overcomplicate it?
Kylie Robson
It’s worth noting that the 90% CI on log-transformed AUC and Cmax is a geometric mean ratio - not arithmetic - which is critical because drug absorption follows first-order kinetics. The 80-125% range was derived from a meta-analysis of over 1,200 bioequivalence studies published between 1980 and 2000, and it correlates tightly with clinical outcomes in over 97% of cases. The FDA doesn’t wing it - they model it with Monte Carlo simulations. Also - Cmax is more variable than AUC because of gastric emptying dynamics. You’re welcome.
Paula Alencar
My heart goes out to anyone who’s ever felt betrayed by a generic pill. I’ve had patients cry in my office because they lost their energy, their focus, their sense of self after switching - and no one listened. The science says it’s fine. But science doesn’t feel the fatigue. It doesn’t hear the racing heart at 3 a.m. The 80/125 rule is a statistical comfort blanket - not a biological guarantee. We need to stop pretending that all drugs are created equal. Some people’s bodies are more sensitive. Some lives hang in the balance. And we owe them more than a confidence interval.
Nikki Thames
It’s not just about the drug - it’s about the person. If you’re the type who obsesses over every little change in your body, you’ll find something wrong with anything. Generics are fine for the rational. But if you’re the type who reads every ingredient label like a sacred text, then maybe you should stick with brand - not because it’s better, but because your mind needs the placebo. And that’s okay. Just don’t pretend your anxiety is pharmacokinetics.
Chris Garcia
In Nigeria, we call generics ‘the people’s medicine’ - and rightly so. When your child needs antibiotics and you have 50 naira in your pocket, you don’t ask if it’s brand or generic - you take it. And guess what? They heal. The West overthinks everything. Bioavailability? Bioequivalence? These are beautiful words - but in the real world, survival is simpler. A pill that works is a pill that works - no matter the label. Let the regulators do their math. Let the people take their medicine.
James Bowers
Anyone who claims generics are unsafe is either misinformed or dangerously naive. The FDA doesn’t approve drugs based on feelings. They approve them based on data - hard, replicable, peer-reviewed data. If you’re experiencing side effects, it’s not the generic. It’s your body. Or your adherence. Or your doctor’s dosing. Stop blaming the pill. Take responsibility.
Will Neitzer
I appreciate the depth of this post - and I want to emphasize that bioequivalence is not about perfection. It’s about predictability. The 80-125% range was chosen because, across thousands of studies, it reliably predicts therapeutic equivalence. The system isn’t broken - it’s brilliant. And for patients who report changes? We don’t dismiss them. We investigate. We check levels. We switch back. We listen. That’s the difference between a bureaucratic process and a medical one.
Gerald Tardif
Look - I’ve been prescribing generics since day one. I’ve had patients swear up and down they ‘feel’ the difference. I’ve had them switch back. I’ve had them switch again. Nine times out of ten? No change in labs. No change in symptoms. But that one time? That one patient who wakes up shaky and cold? I don’t argue. I don’t lecture. I just say - ‘Let’s try the brand again for a month.’ Sometimes, it’s not about the drug. It’s about the trust. And trust matters more than we admit.
Monika Naumann
India has been producing high-quality generics for decades - and yet, Western nations still question our standards. This is not science - it is cultural bias. Our manufacturing facilities meet WHO-GMP, EMA, and FDA standards. We export to the U.S., Europe, and Africa. If your body reacts to a generic, it is not because our pills are inferior - it is because your system is fragile. We do not coddle. We produce. And the world benefits.