By 2025, the world will spend over $1.6 trillion on medicines. That’s more than the entire GDP of Canada. And yet, billions of people still can’t afford the drugs they need. The reason? A broken system where brand-name drugs keep getting more expensive - while generics, the quiet heroes of global health, are the only thing holding the line.
Generics Are the Reason Drug Prices Haven’t Exploded Even Further
Think about this: in the U.S., prescription drug spending jumped from $437 billion in 2023 to $487 billion in 2024. That’s a $50 billion increase in just one year. But here’s the catch - without generics, that number could have been $700 billion. Generics make up 90% of all prescriptions filled in countries like the U.S., Germany, and Japan. Yet they cost only 10-20% of what brand-name drugs do. That’s not a small difference. It’s the difference between someone taking their blood pressure medicine or skipping doses because they can’t pay.
When a patent expires on a drug like Lipitor or Humira, dozens of generic manufacturers jump in. Prices drop fast - sometimes by 80% within months. In India and Thailand, generic versions of HIV and hepatitis C drugs brought treatment costs down from $10,000 a year to under $100. Millions stayed alive because of that price drop. That’s the power of generics.
Why Some Countries Still Can’t Access Them
But not every country benefits equally. In 55 countries, people pay for healthcare out of their own pockets - no insurance, no safety net. In Turkmenistan, Afghanistan, and Nigeria, out-of-pocket spending makes up more than 75% of total health costs. Even if a generic drug costs $2 a month, that’s still too much if you’re living on $2 a day.
And it’s not just about price. In many low-income countries, the supply chain for generics is broken. Pharmacies don’t stock them. Clinics don’t have them. Even when they’re available, people don’t trust them because they’ve been sold fake medicines before. A 2022 WHO report found that 1 in 10 medical products in low- and middle-income countries are substandard or falsified. That erodes trust - and keeps people from using generics even when they’re safe and affordable.
The U.S. Is an Odd Case: High Spending, Low Generic Use in Key Areas
The U.S. spends more on healthcare than any other country - $5.6 trillion in 2025, and climbing to $8.6 trillion by 2033. But here’s the paradox: even with the world’s most advanced generics market, drug spending is still rising fast. Why? Because the most expensive drugs aren’t the ones generics can touch.
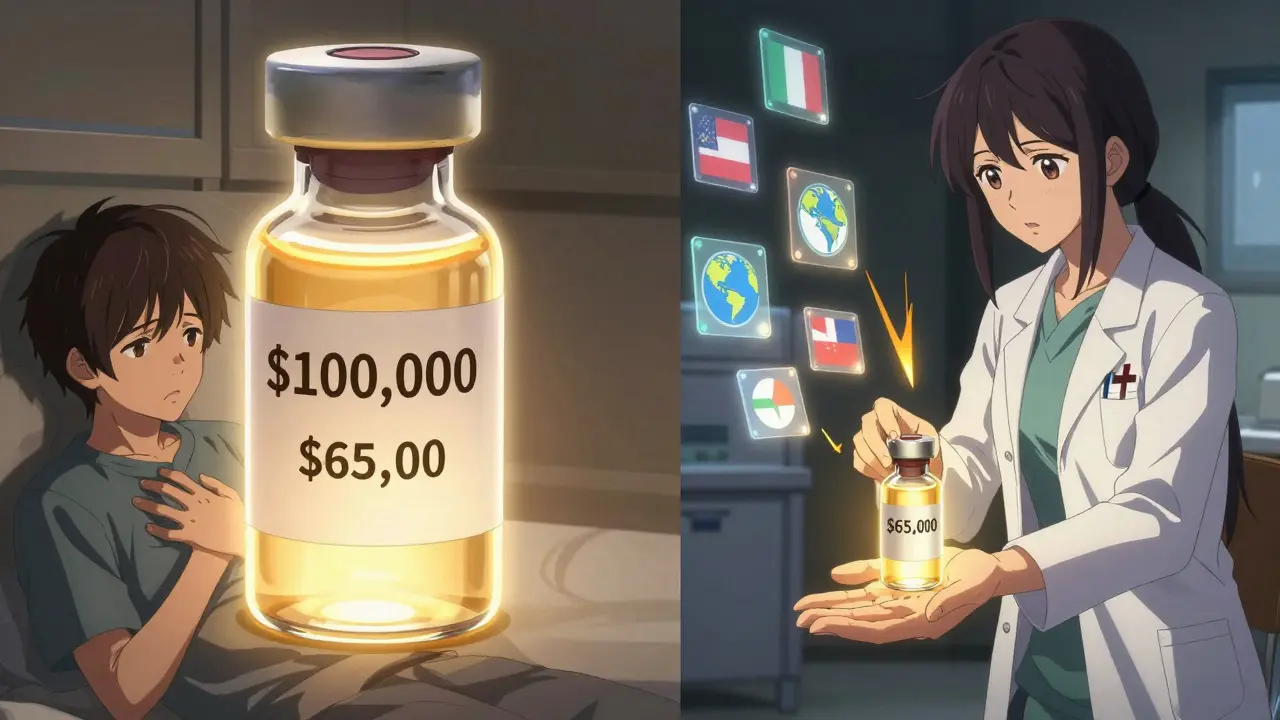
Biologics - complex drugs made from living cells - are the new frontier. Drugs for cancer, rheumatoid arthritis, and diabetes are often biologics. They cost $100,000 a year. And while biosimilars (generic versions of biologics) exist, they’re slow to catch on. Doctors are hesitant to switch. Insurers don’t push them hard enough. In 2024, only 1 in 5 biologic prescriptions in the U.S. were filled with a biosimilar. That’s not because they don’t work - it’s because the system doesn’t reward switching.
Meanwhile, out-of-pocket costs for prescriptions are rising. The average American will pay $231 per person for drugs by 2033 - up from $177 in 2025. That’s a 30% jump. Generics help, but they can’t fix a system where even the cheapest drugs are priced beyond reach for millions.
Emerging Markets Are Changing the Game
While the U.S. struggles with high-cost biologics, countries like China and Brazil are seeing a different trend. After years of relying almost entirely on generics, they’re now adopting more innovative, brand-name drugs. Why? Because their economies are growing. More people have insurance. More clinics are built. And as incomes rise, so does demand for the latest treatments.
But that doesn’t mean generics are disappearing. In fact, they’re becoming more strategic. In China, the government now uses generics to control costs in public hospitals - while allowing brand-name drugs to be sold in private clinics. It’s a two-tier system: generics for the masses, innovators for those who can pay. It’s not perfect, but it’s a pragmatic balance.
India, meanwhile, remains the world’s pharmacy. It produces over 20% of all generic medicines globally. Its manufacturers supply 40% of the U.S. generic market. Yet India itself has a huge access gap. Millions still can’t get basic medicines because distribution is weak and prices - even for generics - are still too high for the poorest.
Why Biosimilars Are the Next Big Battle
The next wave of cost savings isn’t in pills - it’s in injectables. Biosimilars are the generic version of biologic drugs. They’re harder to make, harder to approve, and harder to get doctors to prescribe. But they’re also 15-35% cheaper than the original.
In Europe, biosimilars are widely used. In the U.S., adoption is lagging. Why? Because drug companies pay doctors to keep prescribing the brand. They sue generic makers over patents. They offer rebates to insurers that lock out competitors. It’s legal. It’s profitable. And it’s keeping prices high.
But change is coming. In 2025, over 20 major biologics will lose patent protection. If regulators and insurers act fast, biosimilars could save the global health system over $100 billion in the next decade. But if they don’t - if the same tactics that blocked generics in the 2000s are used again - we’ll be stuck paying $100,000 a year for cancer drugs when $70,000 versions could work just as well.

The Real Cost of Not Using Generics
It’s easy to think of generics as just cheaper pills. But their real value is in keeping entire health systems from collapsing.
In 2022, the global average for public healthcare spending was just 3.8% of GDP. High-income countries hit 5.8%. Low-income countries? 1.2%. That’s not enough to cover even basic care - let alone expensive new drugs. Generics are the reason any care at all is possible in places like Malawi or Haiti. When public budgets shrink - as they did in Lebanon (down 71% since 2019) or Malawi (down 41%) - generics are the only thing that keeps clinics open.
And it’s not just about money. When people can’t afford their meds, they skip doses. Their conditions worsen. They end up in the hospital. That costs more. Generics break that cycle. A diabetes patient on a $5-a-month generic metformin tablet is far less likely to need dialysis or an amputation than one who can’t afford the $200 brand-name version.
What Needs to Change
Generics aren’t a magic fix - but they’re the most powerful tool we have to make healthcare affordable. Here’s what needs to happen:
- Regulators must speed up approval - Generic drug applications take years in some countries. In the U.S., the FDA approved over 1,000 generics in 2024 alone - but many still wait too long.
- Insurers must prioritize generics - If a generic exists, it should be the first option covered. Not the last.
- Doctors must be trained to prescribe them - Many still believe generics are “weaker.” They’re not. They’re identical in active ingredients.
- Supply chains must be strengthened - Especially in Africa and South Asia. No point having cheap drugs if they never reach the pharmacy.
- Patent abuse must be stopped - Drug companies can’t keep extending patents through tiny changes just to block generics.
The truth is simple: if we want healthcare to be accessible, we need generics. Not as a last resort. Not as a charity. But as the foundation.
What’s Next for Global Health Spending?
By 2030, global healthcare spending will likely top $10 trillion. And unless we fix how we pay for drugs, it will keep rising. Generics won’t stop innovation. They’ll make it sustainable. They’ll let us treat more people with less money. They’ll let low-income countries build health systems without going bankrupt.
The question isn’t whether we can afford generics. It’s whether we can afford not to use them.




Comments (13)
Ellie Stretshberry
generics are literally lifesavers and no one talks about it like it’s normal
christian ebongue
lol the pharma execs are out here playing monopoly with people’s kidneys
Joanne Smith
the fact that we treat medicine like a luxury good instead of a basic human right is the real crime here. generics aren’t just cheaper-they’re justice. and yet we still act like they’re some kind of second-class option. sad.
jesse chen
you know what’s wild? the active ingredient in a generic is identical to the brand name. same chemistry. same effect. same safety profile. but doctors still say ‘I’d rather prescribe the original’ like it’s a status symbol. it’s not medicine-it’s branding.
Ryan Cheng
in india, generics are everywhere. my cousin in Bangalore gets his insulin for $3 a month. here in the US, I paid $400 for the same thing last month. we’re not broken because we lack innovation-we’re broken because we chose profit over people.
Prasanthi Kontemukkala
as someone from india, i’ve seen this firsthand. our factories ship billions of pills worldwide-but at home, rural clinics still run out. it’s not that we can’t make them. it’s that the last mile never gets funded. logistics matter as much as price.
Lori Anne Franklin
my grandma took her blood pressure med for 12 years-generic lisinopril, $4 a month. when they tried switching her to the brand, she cried because she couldn’t afford it. she didn’t know the science. she just knew she’d be dead without it.
Jeanette Jeffrey
oh wow another ‘generics are heroes’ essay. let me guess-you’ve never had a drug fail on you? because sometimes generics have batch issues. not all are created equal. stop romanticizing them like they’re magic fairy dust.
Sarah Holmes
It is, of course, entirely unsurprising that a society which commodifies human life would also commodify its most basic medical necessities. The notion that a pharmaceutical patent-a legal fiction-should hold precedence over the biological imperative of survival is not merely unethical; it is ontologically bankrupt. We are not consumers of medicine. We are its subjects. And the system has turned us into liabilities.
Jody Kennedy
you’re right, Jeanette-some generics DO have issues. but that’s because of poor regulation, not the concept. fix the oversight, don’t throw out the baby with the bathwater. we’ve got the tech to test every batch. we just don’t have the will.
Bryan Woods
the biosimilar gap is terrifying. we’ve got drugs that cost $100k a year and we’re not even trying to replace them with 30% cheaper versions. it’s not about science-it’s about who owns the contract.
wendy parrales fong
i’ve worked in clinics in rural america. people skip doses, split pills, go without. not because they’re careless-they’re just broke. generics don’t fix poverty. but they stop poverty from killing people faster.
Alex Ragen
the real tragedy? the same people who scream about ‘socialized medicine’ are the ones who benefit most from generics. they just don’t realize their life is being saved by a system they claim to hate.