Hormone Therapy Decision Guide
Select Patient Characteristics
Recommended Therapy Options
Detailed Comparison Table
| Drug | Class | Primary Indication | Pros | Cons |
|---|
Quick Take
- Tamoxifen remains the go‑to SERM for many estrogen‑driven breast cancers, but it isn’t the only option.
- Raloxifene offers similar estrogen‑blocking effects with a lower risk of uterine cancer.
- Aromatase inhibitors (Anastrozole, Letrozole, Exemestane) shut down estrogen production entirely - best for post‑menopausal patients.
- Fulvestrant is a SERD that destroys the estrogen receptor, useful after SERM failure.
- Choosing the right drug depends on menopausal status, side‑effect tolerance, and specific treatment goals.
When doctors talk about “hormone therapy” for estrogen‑responsive breast cancer, Tamoxifen (brand name Nolvadex) usually gets the spotlight. That’s because it’s been around for decades, is cheap, and works well for many patients. But the landscape has broadened. Newer SERMs, aromatase inhibitors, and even drugs that degrade the estrogen receptor (SERDs) show comparable or better outcomes in certain groups. This article breaks down the science, the pros and cons, and the scenarios where an alternative might beat Tamoxifen.
What is Tamoxifen (Nolvadex)?
When treating estrogen‑responsive breast cancer, Tamoxifen is a selective estrogen receptor modulator (SERM) that blocks estrogen’s action in breast tissue while acting like estrogen in bone and the uterus. Approved by the FDA in 1977, it’s prescribed both as adjuvant therapy after surgery and as a preventive measure for high‑risk women.
How Tamoxifen Works
Tamoxifen binds to estrogen receptors (ERα and ERβ) and prevents estrogen from docking. In breast cells this stops the growth signal, but in bone it mimics estrogen, helping maintain density. In the uterus, however, it can act like estrogen, which explains the small increase in endometrial cancer risk.
Key Benefits and Common Side Effects
- Benefits: Reduces breast cancer recurrence by 40‑50% when used for 5‑10years. Lowers risk of new breast cancers in high‑risk women.
- Hot flashes: Reported by up to 70% of patients, especially during the first six months.
- Thromboembolic events: Deep‑vein thrombosis risk rises to roughly 1‑2per 1,000 patient‑years.
- Uterine effects: Small absolute increase in endometrial hyperplasia and cancer (about 0.5% over 5years).
- Bone health: Acts protectively, often improving bone mineral density.
When Tamoxifen Is Typically Used
It shines in three main scenarios:
- Early‑stage, ER‑positive invasive breast cancer (adjuvant setting).
- Premenopausal women who need hormone therapy but cannot tolerate an aromatase inhibitor.
- Risk‑reduction for women with a strong family history or known BRCA mutations.
For post‑menopausal patients, guidelines now often recommend an aromatase inhibitor (AI) first because of better disease‑free survival, reserving Tamoxifen for special cases.

Alternative Hormone Therapies - An Overview
Alternatives fall into three broad classes:
- Other SERMs - Raloxifene, Clomiphene.
- Aromatase inhibitors (AIs) - Anastrozole, Letrozole, Exemestane.
- Selective estrogen receptor degraders (SERDs) - Fulvestrant.
Each class has its own mechanism, dosing schedule, and side‑effect profile. The table below lines them up side‑by‑side.
| Drug | Class | Primary Indication | Mechanism | Typical Dose | Pros | Cons |
|---|---|---|---|---|---|---|
| Tamoxifen | SERM | Adjuvant & preventive ER‑positive breast cancer | Blocks estrogen receptors in breast, agonist in bone & uterus | 20mg daily, oral | Well‑studied, inexpensive, bone‑protective | Hot flashes, VTE, uterine cancer risk |
| Raloxifene | SERM | Osteoporosis prevention, breast cancer risk reduction | Antagonist in breast, agonist in bone, neutral in uterus | 60mg daily, oral | Lower uterine cancer risk, improves bone density | Less effective as adjuvant therapy, similar VTE risk |
| Anastrozole | Aromatase Inhibitor | Post‑menopausal ER‑positive breast cancer | Inhibits aromatase → ↓ estrogen synthesis | 1mg daily, oral | Higher disease‑free survival, no uterine stimulation | Joint pain, bone loss, cardiovascular profile |
| Letrozole | Aromatase Inhibitor | Adjuvant & metastatic breast cancer (post‑menopausal) | Potent aromatase blockade | 2.5mg daily, oral | Strong estrogen suppression, proven OS benefit | Severe arthralgia, osteoporosis risk |
| Exemestane | Aromatase Inhibitor (steroidal) | Sequential therapy after 5‑year Tamoxifen | Irreversible aromatase inhibition | 25mg daily, oral | May cause less joint pain than non‑steroidal AIs | Weight gain, hot flashes, bone loss |
| Fulvestrant | SERD | Metastatic ER‑positive breast cancer (post‑menopausal) | Destroys estrogen receptor, no agonist activity | 500mg IM injection monthly (loading schedule) | Effective after SERM failure, no uterine effects | Injection site pain, liver enzyme rise, cost |
| Clomiphene | SERM (fertility) | Infertility due to anovulation, off‑label breast cancer | Partial estrogen agonist → ↑ gonadotropins | 25‑100mg daily, oral (cycles) | Useful in pre‑menopausal women needing ovulation induction | Visual disturbances, ovarian cysts, limited breast cancer data |
Deep Dive Into the Main Alternatives
Raloxifene - The Bone‑Friendly SERM
Raloxifene is a selective estrogen receptor modulator approved for osteoporosis prevention and for reducing invasive breast cancer risk in post‑menopausal women. Unlike Tamoxifen, it does not stimulate the uterine lining, so the endometrial cancer risk is essentially zero. Its side‑effect profile mirrors Tamoxifen’s hot flashes and VTE risk, but many patients tolerate it better because bone health improves.
Fulvestrant - The Pure Antagonist
Fulvestrant is a selective estrogen receptor degrader (SERD) that binds, folds, and destroys the estrogen receptor, eliminating any residual estrogen signaling. It’s given as a deep intramuscular injection-500mg on days 0, 14, 28, then monthly. Clinical trials (e.g., CONFIRM) show it can extend progression‑free survival after Tamoxifen or AI failure. The trade‑off is the injection schedule and higher cost.
Aromatase Inhibitors - Cutting the Supply Line
The three most common AIs-Anastrozole, Letrozole, and Exemestane-all block the aromatase enzyme that converts androstenedione to estrogen. They are only effective after menopause, when peripheral conversion is the main estrogen source. Studies (ATAC, BIG 1‑98) demonstrate a modest but clear advantage in disease‑free survival over Tamoxifen for post‑menopausal patients.
Side effects lean toward musculoskeletal pain and bone density loss, so regular DEXA scans and calcium/vitaminD supplementation are standard.
Clomiphene - The Fertility‑Focused SERM
Clomiphene works by blocking estrogen feedback at the hypothalamus, leading to a surge in follicle‑stimulating hormone (FSH) and ovulation. While not a primary breast‑cancer drug, it’s occasionally used off‑label in pre‑menopausal patients who need a SERM but also desire fertility preservation. Limited data suggest a neutral impact on breast cancer outcomes, but the visual side effects and ovarian cyst risk keep it from mainstream use.
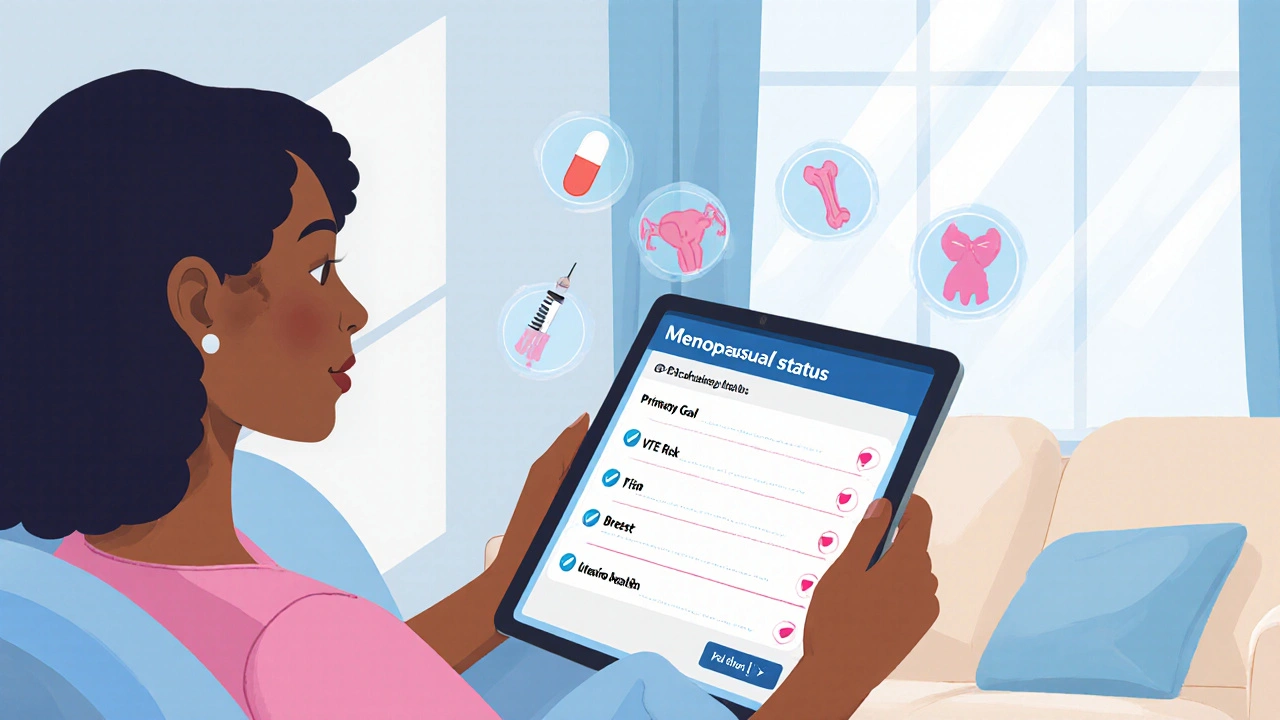
Decision Criteria - How to Pick the Right Drug
Ask yourself these five questions before settling on a regimen:
- Is the patient pre‑ or post‑menopausal? AIs are off the table for pre‑menopausal patients.
- What is the primary goal? Adjuvant cure, risk reduction, or bone health?
- How does the patient tolerate hot flashes or joint pain?
- Is there a history of uterine issues or VTE?
- Are cost and administration route (pill vs. injection) major factors?
Based on the answers, you can narrow the field:
- Pre‑menopausal, low VTE risk: Tamoxifen or Clomiphene (if fertility matters).
- Post‑menopausal, focus on bone health: Raloxifene or switch to an AI with concurrent bisphosphonate.
- Progression after a SERM: Move to a SERD like Fulvestrant or an AI.
Monitoring and Managing Side Effects
Regardless of the chosen drug, regular follow‑up is key:
- Baseline and annual mammograms.
- DEXA scan at baseline and every 2‑3years if on an AI.
- Blood work every 6months (CBC, liver enzymes for Fulvestrant, lipid profile for AIs).
- Patient‑reported outcome tools for hot flashes and joint pain-adjust dose or add gabapentin/clonidine if needed.
If a VTE event occurs, pause the SERM/AIs and switch to anticoagulation, then consider moving to a different class after recovery.
Frequently Asked Questions
Can I switch from Tamoxifen to an aromatase inhibitor after a few years?
Yes. Many clinicians use a “switch strategy”: Tamoxifen for 2‑3years followed by an AI for the remainder of a 5‑year course. This can reduce the cumulative risk of uterine side effects while preserving the estrogen‑blocking benefit.
Is Raloxifene as effective as Tamoxifen for preventing breast cancer?
In the STAR trial, Raloxifene lowered invasive breast cancer incidence by about 38% compared with placebo, similar to Tamoxifen, but it did not reduce non‑invasive disease as much. The advantage is a lower uterine cancer risk, making it a solid option for women with a uterus who are concerned about that side effect.
Do aromatase inhibitors cause menopausal symptoms?
AIs can trigger hot flashes, night sweats, and mood swings because they abruptly cut estrogen production. However, these symptoms are often milder than those seen with SERMs. Managing them with lifestyle tweaks or low‑dose SSRIs is common practice.
What’s the biggest drawback of Fulvestrant?
The injection schedule is inconvenient (monthly deep intramuscular shots) and the drug is pricey. Some patients also experience liver enzyme elevations, so regular LFT monitoring is advised.
Can I take a SERM and an AI together?
Combining them offers no added benefit and can increase toxicity. Guidelines recommend using one class at a time, switching only when treatment goals change or side effects become intolerable.
Next Steps for Patients and Clinicians
If you’re starting hormone therapy, schedule a baseline assessment (mammogram, DEXA, labs). Discuss menopausal status, risk tolerance, and lifestyle preferences. Choose the drug that aligns with the decision matrix above, then set up a monitoring calendar-usually every 3‑6months for the first year, then annually if stable.
For clinicians, keep an eye on emerging data from CDK4/6 inhibitor combinations with AIs-they’re reshaping first‑line therapy in 2024‑2025. While not a direct alternative to Tamoxifen, they illustrate how hormone manipulation continues to evolve.



Comments (17)
Nicole Chabot
Interesting breakdown, especially the bone‑protective angle of Tamoxifen.
Sandra Maurais
While the data is thorough, the omission of cost‑effectiveness analysis feels like a glaring oversight. 💰📉
Michelle Adamick
Great dive! The pharmacodynamics of SERMs vs. AIs can be a real game‑changer for patient‑centred care 🚀🧬. Let’s not forget the impact on micro‑metastatic niches when we switch modalities.
Edward Glasscote
Looks solid, though I wonder how often clinicians actually follow the decision matrix in a busy clinic.
Gaurav Joshi
Honestly, all these drugs are just different flavors of the same estrogen blockade; the hype around “newer is better” is overrated.
Jennifer Castaneda
The pharmaceutical industry isn’t just selling drugs; they’re selling a narrative that keeps us dependent on ever‑changing regimens, all while monitoring our every health metric for data mining.
Annie Eun
Fascinating read! The interplay between menopausal status and drug choice truly underscores the need for personalized therapy.
Jay Kay
TL;DR: Tamoxifen cheap good bone, AIs better outcomes post‑menopause, watch VTE, think cost.
Franco WR
Reading through this guide reminded me how nuanced hormone therapy truly is, and it’s worth unpacking each point in detail.
First, the historical context of Tamoxifen shows why it remains a reference point; decades of data provide a safety net that newer agents haven’t yet built.
Second, the bone‑protective effect of Tamoxifen can't be overstated, especially for pre‑menopausal patients who are at risk of early osteopenia.
Third, the VTE risk, while low in absolute terms, becomes clinically relevant when patients have additional thrombophilia factors, necessitating a thorough risk assessment.
Fourth, the uterine stimulation issue demands vigilance; regular endometrial monitoring should be standard for any long‑term Tamoxifen user.
Fifth, Raloxifene’s neutral uterine profile makes it an attractive alternative for women with a history of endometrial hyperplasia, yet its modest efficacy in the adjuvant setting may limit its use when cure is the primary goal.
Sixth, aromatase inhibitors such as Anastrozole and Letrozole deliver superior disease‑free survival for post‑menopausal patients, but they introduce musculoskeletal pain and bone loss that often require bisphosphonate co‑therapy.
Seventh, the newer steroidal AI, Exemestane, may reduce joint pain compared with non‑steroidal options, though the data are still mixed and cost remains a barrier.
Eighth, Fulvestrant’s mechanism of degrading the estrogen receptor offers a powerful option after SERM or AI failure, but its injectable form and cost make it less convenient for many patients.
Ninth, patient preference for oral versus injectable routes is a practical consideration that can affect adherence; some patients may prefer the monthly injection despite the inconvenience because it removes daily pill fatigue.
Tenth, monitoring schedules-regular mammograms, DEXA scans, and liver panels-are essential regardless of the chosen agent to catch adverse effects early.
Eleventh, emerging data on CDK4/6 inhibitors combined with AIs suggest a future shift in first‑line therapy, highlighting the importance of staying updated with trial results.
Twelfth, cost‑effectiveness analyses remain crucial; while Tamoxifen is inexpensive, newer agents may be justified in high‑risk populations if they significantly improve outcomes.
Thirteenth, shared decision‑making, incorporating patient values, side‑effect tolerance, and lifestyle, ultimately drives the best therapeutic choice.
Fourteenth, clinicians should remain flexible, ready to switch strategies-such as the “Tamoxifen‑to‑AI” switch-based on evolving risk profiles.
Fifteenth, overall, this guide serves as a valuable decision aid, but the real world demands individualized assessment beyond algorithmic recommendations.
Rachelle Dodge
Colorful and concise: pick the drug that sings with your patient’s life rhythm.
Gaurav Joshi
While the contrarian view raises a point, it’s essential to balance novelty with evidence‑based outcomes.
Elaine Proffitt
Agree with the need for cost analysis; without it, the guide feels incomplete.
Christopher Munt
Appreciate the thoroughness; I’d add that patient education on hot flashes can improve adherence 😊.
Mike Creighton
The drama of clinical decision‑making is akin to a chess match; each move-be it Tamoxifen or an AI-carries strategic weight in the battle against cancer.
Desiree Young
Is it just me or does the industry push these drugs like they're the only hope?
Kaustubh Panat
One must acknowledge the intellectual rigor behind these therapeutic pathways, though the layman often overlooks the subtle pharmacologic elegance.
Arjun Premnath
Great summary! Keeping a positive outlook while monitoring side effects can really empower patients.