Every year, millions of people in the U.S. take their medicine wrong-not because they’re careless, but because the label on their pill bottle doesn’t make sense. You might think you know what "take twice daily" means. But if you’re not sure whether that means every 12 hours or just morning and night, you’re not alone. And that confusion can land you in the emergency room.
Why Prescription Labels Are So Hard to Understand
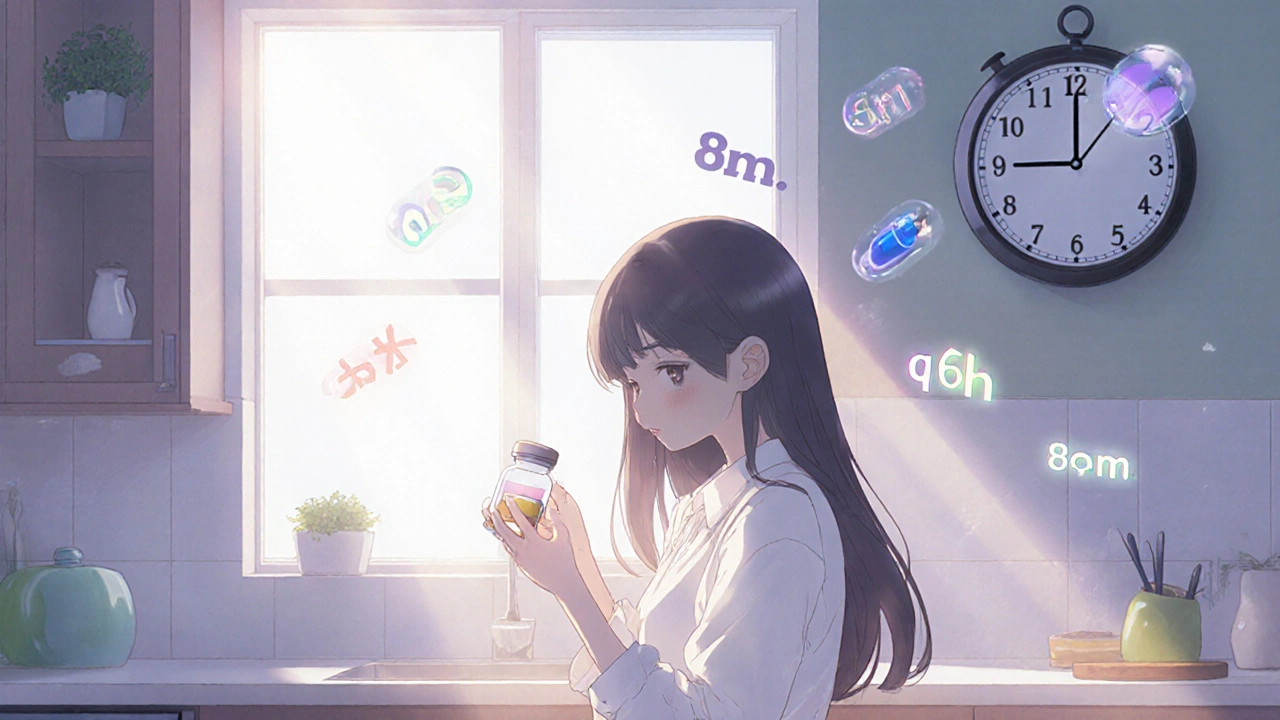
Prescription labels weren’t designed for real people. They were built for pharmacists, using shorthand like "q6h," "BID," or "PO." These terms are standard in medical training, but they’re meaningless to most patients. A 2006 study found that 46% of adults misunderstood at least one instruction on their prescription label. That number jumps to 71% for people with low health literacy. Even simple phrases cause problems. "Take with food" doesn’t mean "take instead of food." Many patients skip meals to take their pills, thinking that’s what the label wants. Others take their antibiotic every two hours because they think "four times a day" means every six hours-24 divided by 4 is 6, right? One Reddit user shared how he took his antibiotic four times a day for three days, thinking "q6h" meant four doses. He ended up in the ER with stomach bleeding. The language on labels is often too complex. Over 27% of instructions are written at a reading level higher than high school. That’s not just a problem for older adults or non-native speakers. Even college-educated patients get it wrong. One study showed 23% of people with good literacy misunderstood basic directions like "take once daily."Top 5 Prescription Label Mistakes Patients Make
- "Take once daily" vs. "Take once" - Some patients think "take once" means take it one time total, not every day. They stop after the first dose.
- "Twice daily" means every two hours - Many assume "twice daily" means every 12 hours, but others think it means every two hours, leading to dangerous overdoses.
- "Take with food" = "take instead of food" - Patients skip meals to take pills, thinking they’re following instructions. This can reduce absorption or cause nausea.
- "As needed" means "whenever I feel like it" - Painkillers or sleep aids labeled "as needed" are often taken too frequently, leading to dependency or overdose.
- Ignoring warning icons - A symbol for "avoid alcohol" or "may cause drowsiness" looks like a cartoon to many. A 2021 FDA test found 68% of patients misinterpreted the "take with food" icon.
What Makes a Prescription Label Actually Work?
The best labels don’t use jargon. They use plain language. Instead of "ii tab PO qHS," they say: "Take 2 tablets by mouth at bedtime." That’s the kind of clarity the U.S. Pharmacopeia (USP) recommends-and it works. Studies show labels written this way cut misunderstanding rates from 46% to just 12%. Effective labels follow three rules:- Use active voice: "Take 1 tablet daily" is clearer than "One tablet should be taken daily."
- Limit steps: One or two instructions max. Don’t cram 5 directions onto one line.
- Use familiar words: "Morning" and "evening" are better than "BID." "At bedtime" is better than "qHS."
How Pharmacies Are (and Aren’t) Fixing This
Some pharmacies are making real changes. CVS, Walgreens, and Walmart now use clearer label templates called "ClearView" or "SimpleScript." These labels use larger fonts (12pt minimum), high-contrast colors, and visual cues like clock icons showing 8 a.m. and 8 p.m. for twice-daily doses. But not all pharmacies are on the same page. Independent pharmacies often use older systems that haven’t been updated. A 2023 survey found only 32% of independent pharmacies follow USP Chapter <17> standards, compared to 78% of big chains. That means your medication might be safer at CVS than at your local mom-and-pop pharmacy-even if they’re filling the same prescription. The problem is money. Updating pharmacy software costs $2,500 to $5,000 per location. Many small pharmacies can’t afford it. And even when they do, staff aren’t always trained to explain the labels. That’s why the "Teach-Back" method matters. When a pharmacist asks, "Can you tell me when you’ll take this pill?" and the patient says, "Every morning and night," that’s proof they understood. Studies show this simple check reduces errors by 58%.What You Can Do Right Now
You don’t have to wait for pharmacies to fix this. Here’s what you can do the next time you get a prescription:- Ask for a plain-language label. Say: "Can you print this in simple words? I want to make sure I take it right."
- Request visual aids. Ask for a clock icon showing when to take it. Many pharmacies can add this.
- Use the "Teach-Back" trick. After the pharmacist explains, say: "Just to make sure I got it-so I take one pill at 8 a.m. and another at 8 p.m.?" If they say yes, you’re good.
- Check the font size. If you can’t read it without squinting, ask for a large-print version. All major chains offer this for free.
- Use a pill organizer. 78% of patients who use one say it helps them avoid mistakes. You can get free ones at pharmacies or online.
- Download a label helper app. GoodRx’s "Label Lens" app lets you scan your label and get a plain-language translation. It’s free and works with 89% accuracy.
Language Barriers and Special Populations
Spanish-speaking patients face extra challenges. Only 12% of U.S. pharmacies offer labels in Spanish-even though 41 million Americans speak Spanish at home. And when labels are translated, they’re often done poorly. A 2015 study found Spanish labels had inconsistent terms like "con comida" vs. "durante las comidas," confusing patients even more. Seniors are another high-risk group. One in three Medicare beneficiaries skip doses because they don’t understand the instructions. For people with memory problems or dementia, even perfect labels aren’t enough. That’s why family members or caregivers should be involved in the pharmacy visit.The Future of Prescription Labels
New tech is coming. By January 1, 2025, USP will require QR codes on all prescription labels. Scan it, and you’ll see a video or pictogram showing exactly how to take the medicine. Mayo Clinic’s pilot program saw a 62% drop in errors after adding QR codes. Amazon Pharmacy now offers voice-enabled labels. Say, "Hey Amazon, how do I take this?" and it reads the instructions aloud. Early tests showed a 38% drop in senior errors. The government is pushing for change too. The Biden administration allocated $200 million to improve health literacy through 2026. Seventeen states are passing laws to require plain-language labels by 2025. If federal rules follow, we could see a 44% drop in label-related errors by 2030. But progress won’t happen unless patients speak up. If your label doesn’t make sense, say so. Ask for help. Demand clarity. Your life could depend on it.What does "BID" mean on a prescription label?
"BID" stands for "bis in die," which is Latin for "twice a day." But most patients don’t know that. Instead of "BID," the label should say: "Take 1 tablet two times each day-once in the morning and once in the evening." Always ask your pharmacist to explain any abbreviations.
Can I just take my pill whenever I remember?
Only if the label says "as needed." For antibiotics, blood pressure meds, or diabetes drugs, timing matters. Taking them at random times can make them less effective or even dangerous. If the label says "take every 8 hours," you need to space them out evenly. If you’re unsure, call your pharmacy or use a pill reminder app.
Why do some labels say "take with food" and others say "take on an empty stomach"?
Some medicines work better when they’re with food-it helps your body absorb them or stops stomach upset. Others need an empty stomach so food doesn’t block absorption. If you’re not sure, ask your pharmacist: "Should I take this before, during, or after a meal?" Don’t guess.
Are big pharmacies better with labels than small ones?
Yes, generally. Chains like CVS, Walgreens, and Walmart have updated their systems to use clearer, standardized labels. Independent pharmacies often use older software and may still use confusing abbreviations. If you’re unsure, ask if they follow USP Chapter <17> standards-or just request a plain-language version.
What should I do if I think I took my medicine wrong?
Call your pharmacist immediately. They can tell you if it’s dangerous and what to do next. Don’t wait for symptoms. If you took too much, took it at the wrong time, or skipped doses for days, it’s better to be safe. You can also call Poison Control at 1-800-222-1222 for free advice.



Comments (14)
doug schlenker
I used to take my blood pressure med at random times until my grandma told me to write down when I took each pill. Now I use a little notebook and it’s changed everything. No more guessing. Simple, but it works.
Also, I asked my pharmacist for a big-print label last week and they printed it for free. No drama. Just ask.
People think pharmacies are out to confuse you, but most of them want you to be safe. You just gotta speak up.
And yeah, ‘BID’ is Latin. But why should I need a degree in Latin to not die? That’s the real problem.
Skye Hamilton
soooooo... the government wants to add QR codes to pills now? next they’ll be scanning your eyeballs to make sure you’re not faking your headache.
also, ‘take with food’ means take it with a cheeseburger? or just a cracker? why is this so hard? i think they’re all just playing us.
and why do i feel like the real answer is ‘just don’t get sick’?
Austin Simko
Big Pharma owns the pharmacies. The labels are confusing on purpose. They want you to mess up so you come back for more. It’s profit-driven negligence.
QR codes? That’s just surveillance with a side of pills.
Nicola Mari
It’s not the labels. It’s the people. If you can’t follow basic instructions, you shouldn’t be trusted with medication. This isn’t a design flaw-it’s a human failure.
And don’t get me started on the ‘Teach-Back’ nonsense. You’re not a toddler. Read the damn thing.
Also, why are we letting non-native speakers dictate how labels are written? The language is English. Use English.
Sam txf
Let me guess-someone at CVS got a bonus for ‘ClearView’ labels. Meanwhile, your local pharmacy is stuck with 1998 software because they’re too cheap to upgrade.
And don’t even get me started on ‘as needed’ painkillers. People are popping those like Skittles. You think that’s a label problem? Nah. It’s a ‘I don’t care about consequences’ problem.
Fix the people, not the font size.
Leah Doyle
I love that GoodRx has that Label Lens app! I scanned my antibiotic label last month and it said ‘Take every 8 hours, even if you feel better.’ I was taking it ‘twice a day’ because I thought that was enough 😅
Also, my mom’s pharmacist uses a clock icon now-8am and 8pm with little sun and moon. She’s 78 and finally gets it. I cried.
Small changes. Big difference. 💙
Jacob Hepworth-wain
Just asked my pharmacist for a plain-language label yesterday. He printed it out on thicker paper with bigger letters and even drew a little clock. No extra charge. No attitude.
Simple stuff, right? But it’s rare enough that it felt like a win.
Also, pill organizer? Best $3 I ever spent. I used to forget if I took it or not. Now I just look at the slots.
Don’t overthink it. Ask. Use tools. Stay alive.
Craig Hartel
My cousin in India gets her meds from a small clinic and they write everything in Hindi and English side by side-no jargon, just clear words and pictures. It’s beautiful.
Why can’t we do that here? We’ve got the tech. We’ve got the know-how.
It’s not about money. It’s about caring. And honestly? If we treated health like a human right instead of a transaction, labels wouldn’t be the problem.
Keep pushing for change. It matters.
Chris Kahanic
While the intent behind plain-language labeling is commendable, the implementation remains inconsistent across healthcare systems. The variance in pharmacy infrastructure, staff training, and regulatory compliance creates a fragmented patient experience. Standardization, while ideal, requires systemic coordination that is currently lacking.
Moreover, the reliance on technological solutions such as QR codes may inadvertently exclude elderly or low-income populations without smartphones or digital literacy. A multilayered approach-combining human interaction, visual aids, and simplified text-is necessary for equitable outcomes.
Geethu E
I work in a pharmacy in Mumbai and we write everything in simple English and Hindi-no ‘BID’, no ‘qHS’. We draw clocks. We say ‘morning’ and ‘night’. We ask patients to repeat it back. We don’t care if it’s ‘not standard’-we care if they live.
And guess what? Our error rate is lower than most US pharmacies.
It’s not about money. It’s about respect.
Also, if you’re scared to ask, just say ‘I’m not smart enough to understand this’-we’ve heard it all. We won’t judge. We’ll help.
anant ram
Yes, yes, yes! I’ve been saying this for years! People think they’re being ‘efficient’ by using Latin abbreviations, but they’re just being lazy-and it’s costing lives! Every time I see ‘q6h’ on a label, I want to scream!
And the ‘as needed’ thing? That’s a disaster waiting to happen. My uncle took his sleep med 5 times in one night because he thought ‘as needed’ meant ‘whenever I feel like it’-he ended up in the hospital!
Plain language isn’t ‘dumbing down’-it’s saving lives. And if your pharmacy won’t give it to you? Go somewhere else. Your life is worth more than their outdated software.
George Hook
Let’s be honest: this isn’t just about labels. It’s about the entire healthcare system being designed to optimize profit, not patient understanding. We’ve turned medicine into a transactional experience-fast, impersonal, and confusing.
Pharmacies are under pressure to fill prescriptions quickly, so they don’t have time to explain. Doctors are overworked and don’t have time to reinforce instructions. Patients are left in the dark.
QR codes? Voice assistants? These are band-aids on a broken system. What we need is a cultural shift: medicine as a conversation, not a receipt.
And yes, I know this sounds idealistic. But if we keep treating patients like data points, we’ll keep losing people to simple mistakes.
It’s not about making labels prettier. It’s about making people feel seen.
jaya sreeraagam
OMG I JUST REALIZED-my mom’s label said ‘take with food’ and she was taking it with a cup of coffee and a cigarette. She thought ‘food’ meant ‘anything you eat while sitting down’ 😭
She’s 72, has diabetes, and takes 7 meds. She’s terrified of messing up.
So I sat down with her last night and we made a little chart: morning = banana + pill, night = peanut butter toast + pill. We even drew smiley faces.
She cried. I cried.
It’s not about tech. It’s about love. And time. And patience.
And if your pharmacy doesn’t give you that? Find someone who will.
Katrina Sofiya
While I commend the efforts toward improved health literacy, the systemic nature of this issue requires legislative intervention. The current voluntary adoption of plain-language standards by large chains is insufficient. A federal mandate, backed by enforceable compliance standards and funding for small pharmacies, is not merely advisable-it is ethically imperative.
Furthermore, the integration of multilingual labeling and culturally competent communication protocols must be prioritized to serve the diverse population of the United States. Health equity is not a privilege; it is a right.