
Metoclopramide Hiccups Quiz
Metoclopramide is a dopamine antagonist and anti‑emetic approved by the FDA. It blocks dopamine D2 receptors in the chemoreceptor trigger zone and enhances gastrointestinal motility, which is why doctors sometimes reach for it when ordinary hiccup remedies fail.
- Quick snapshot: oral dose 10‑20mg, onset 30‑45minutes, duration 3‑4hours.
- Targeted at persistent (≥48h) or intractable (≥1month) hiccups.
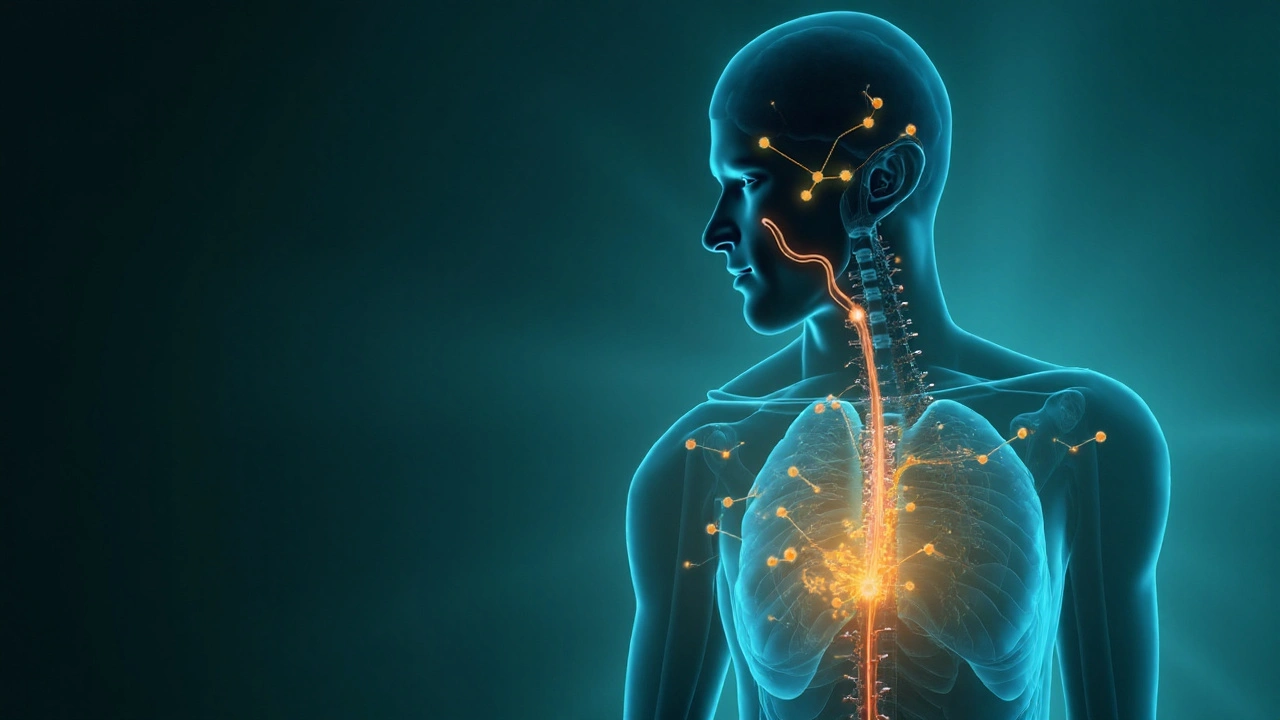
- Works by interrupting the hiccup reflex arc at the brainstem level.
What Triggers Hiccups?
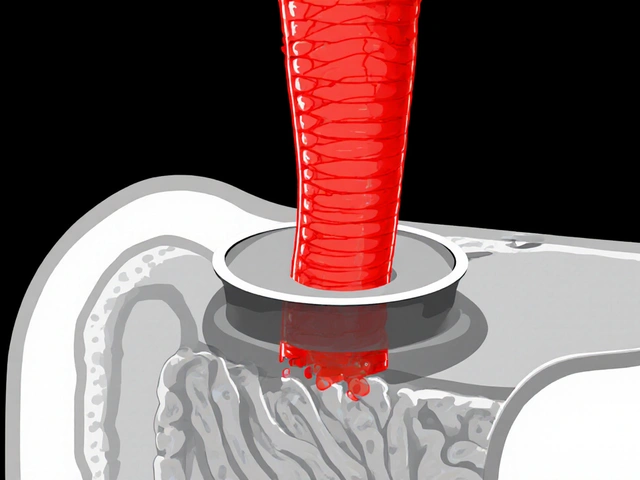
Hiccups, medically termed singultus, arise from a sudden contraction of the diaphragm followed by an abrupt closure of the glottis. Common culprits include rapid eating, carbonated drinks, or a sudden change in temperature. When the spasms linger, they can disrupt sleep, cause fatigue, and even lead to weight loss.
Why a Dopamine Antagonist Helps
The hiccup reflex arc involves the phrenic nerve, vagus nerve, and the central pattern generator in the medulla. Dopamine antagonist activity dampens the excitatory signals in the medulla, effectively “resetting” the rhythm. Metoclopramide’s ability to boost gastric emptying also reduces gastric distention, a known trigger for the reflex.
Clinical Evidence: Do Studies Back It Up?
Several small clinical trials have evaluated metoclopramide for hiccups. A 2018 randomized, double‑blind study of 34 patients with intractable hiccups reported a 70% response rate (defined as >50% reduction in episode frequency) within 24hours of a single 20mg dose. Another 2021 case series involving 12 patients with hiccups secondary to gastroesophageal reflux disease (GERD) found that 9 participants achieved complete remission after a 5‑day course.
While the sample sizes are modest, the consistency across studies suggests genuine efficacy, especially when traditional remedies (water gulping, breath holding) have failed.
Dosage and Administration Guidelines
Standard dosing for hiccups mirrors the anti‑emetic protocol:
- Initial dose: 10mg orally every 6hours.
- If symptoms persist after 48hours, increase to 20mg every 6hours (max 80mg/day).
- Treatment duration should not exceed 7days without specialist review, to limit the risk of tardive dyskinesia.
Patients with renal impairment require dose reduction by 50% because metoclopramide is cleared renally.
Safety Profile and Common Side Effects
Most users tolerate short courses well. The most frequently reported side effects include:
- Drowsiness or fatigue (≈15% of patients).
- Restlessness or akathisia (≈5%).
- Extrapyramidal symptoms, such as mild tremor (rare, <1%).
Long‑term exposure can cause tardive dyskinesia, a potentially irreversible movement disorder. That’s why the drug is generally reserved for brief, targeted use in hiccup management.
How Does Metoclopramide Stack Up Against Other Hiccup Medications?
| Drug | Class | Typical Dose for Hiccups | Onset | Key Side Effects |
|---|---|---|---|---|
| Metoclopramide | Dopamine antagonist | 10‑20mg q6h | 30‑45min | Drowsiness, extrapyramidal symptoms |
| Chlorpromazine | Phenothiazine antipsychotic | 25‑50mg IV/IM | 15‑30min | Hypotension, sedation |
| Baclofen | GABA‑B agonist | 5‑10mg PO q8h | 1‑2h | Muscle weakness, dizziness |
Metoclopramide shines when the hiccups are linked to gastric stasis or when an oral regimen is preferred. Chlorpromazine acts faster intravenously but carries a higher risk of cardiovascular side effects. Baclofen is useful for neurologic‑origin hiccups but may cause muscle fatigue.
Practical Tips for Patients and Clinicians
Before reaching for metoclopramide, confirm that the hiccups are truly persistent. A quick work‑up should rule out:
- Electrolyte imbalances (especially hyponatremia).
- Central nervous system lesions (stroke, tumor).
- Medications that lower the seizure threshold.
If metoclopramide is chosen, advise patients to avoid driving or operating heavy machinery for at least 2hours after the first dose, due to possible drowsiness. Encourage them to report any involuntary facial movements immediately.
Related Concepts and Next Steps
Understanding hiccups opens the door to several adjacent topics. Readers interested in the broader picture might explore:
- The role of gastroesophageal reflux disease in chronic hiccups.
- Non‑pharmacologic maneuvers (vagal stimulation, diaphragmatic breathing).
- When to refer to a neurologist for central‑nervous‑system evaluation.
These pathways help ensure that hiccup management is part of a comprehensive health strategy rather than an isolated quick fix.
Frequently Asked Questions
How fast does metoclopramide stop hiccups?
Most patients notice a reduction in hiccup frequency within 30‑45minutes after the first oral dose. Full remission may take up to 24hours, especially for stubborn cases.
Is metoclopramide safe for children?
The drug is sometimes used off‑label in adolescents, but pediatric dosing must be weight‑adjusted and limited to short courses. Always consult a pediatric specialist before giving it to a child.
Can I combine metoclopramide with other hiccup drugs?
Combining two dopamine antagonists (e.g., metoclopramide + chlorpromazine) isn’t recommended because side‑effect profiles overlap. However, a clinician may switch agents if the first fails.
What are the warning signs of serious side effects?
Watch for involuntary facial movements, tongue protrusion, or persistent tremor-these could signal early tardive dyskinesia. Seek medical help immediately.
Do I need a prescription to get metoclopramide?
Yes, it’s a prescription‑only medication in the United States because of its potential for serious neurologic effects.
Are there any natural alternatives that work as well?
Techniques like slow breathing, sipping cold water, or stimulating the soft palate can help mild bouts, but they haven’t shown the same success for persistent hiccups that metoclopramide does in clinical studies.
What should I do if hiccups return after finishing the course?
Contact your healthcare provider. They may repeat a short tap‑dose, switch to another agent, or investigate underlying conditions that trigger the reflex.




Comments (17)
Ginger Henderson
Honestly? I tried this after two weeks of hiccups and it worked like magic. No more sobbing into my pillow at 3 a.m.
Cynthia Boen
This is why medicine is broken. You give someone a dopamine blocker for hiccups? Next they'll prescribe antipsychotics for sneezing.
Douglas Fisher
I’ve seen this work in the ER… but I’ve also seen the side effects-people pacing the halls like they’re being chased by ghosts. It’s not a party trick. Use it wisely.
Bethany Buckley
The pharmacodynamic modulation of dopaminergic neurotransmission within the medullary reticular formation-when coupled with vagal afferent attenuation-represents a paradigm-shifting intervention in neurogastroenterology. 🌌✨
Stephanie Deschenes
If you’re considering this, please talk to your doctor first. Especially if you’re on other meds or have kidney issues. It’s powerful-but not a quick fix.
Jesús Vásquez pino
You guys are acting like this is some kind of miracle drug. It’s a last-resort medication with serious risks. Why not just try sipping water or holding your breath for once?
hannah mitchell
I had hiccups for 72 hours once. Nothing worked. Then I took metoclopramide. Felt weird for a day, but the hiccups vanished. Worth it.
vikas kumar
In my village in India, we use jaggery and warm water. But if science says this works, then maybe we should listen. No harm in trying both.
Vanessa Carpenter
I’m just glad someone finally wrote about this. I’ve been googling for weeks. Thank you.
Bea Rose
70% response rate? That means 30% of people wasted time, money, and risked side effects. This isn't a cure. It's a gamble.
Michael Collier
The clinical evidence presented, while promising, must be contextualized within the limitations of small-sample, non-generalizable cohorts. Further randomized, multicenter trials are warranted to establish robust efficacy and safety profiles.
Shannon Amos
So… we’re giving people antipsychotics for hiccups now? Cool. Next up: lithium for burping.
stephen riyo
I tried this… and yeah, it worked… but I felt like I was in a zombie movie for 3 hours. Like, my face didn’t move, and I couldn’t stop staring at the wall…
Jaspreet Kaur
Hiccups are the universe whispering that something is out of balance. Metoclopramide silences the whisper. But does it heal the soul?
Gina Banh
The 2021 GERD study? That’s the real story. If your hiccups are from acid reflux, treat the reflux. This is just putting a bandaid on a broken bone.
Deirdre Wilson
I once hiccuped for 11 days. Tried everything-sugar, lemon, scaring myself. Then I took 10mg of this stuff. Felt like my brain hit reset. Hiccups? Gone. Like, poof.
Bea Rose
And yet, doctors still prescribe it like candy. That’s the problem.