
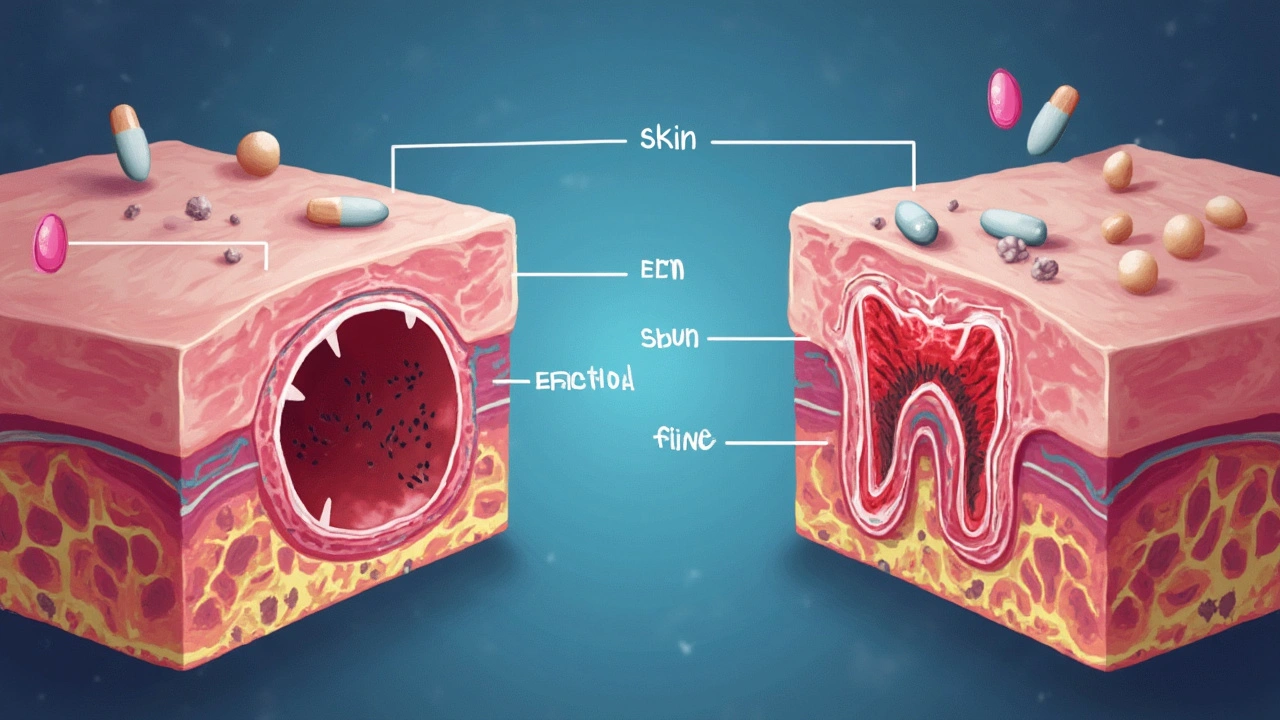
If you’ve ever had a gnarly tooth infection or a stubborn skin boil, there’s a good chance your doctor pulled out clindamycin to fix the mess. This antibiotic has a bit of a tough-guy reputation in the medical world—like the bouncer doctors trust to throw out tough bacteria when others have failed. Some people don’t even know it exists until the amoxicillin stops working. But once you get a taste of how it works, and why doctors save it for the bigger fights, you might look at your antibiotics cabinet pretty differently.
How Clindamycin Works and When Doctors Use It
Clindamycin isn’t your garden-variety antibiotic. People are often surprised to learn it’s actually been around since the 1960s, but doctors still reach for it today because it tackles some of the nastiest bacteria out there. It works by blocking the production of “protein factories” inside bacteria cells—scientists call those ribosomes. Without these, bacteria can’t multiply, and your immune system finally gets a breathing space to win the battle.
You’ll spot clindamycin showing up in the prescription list for everything from dental abscesses to deep bone and joint infections (that’s called osteomyelitis). Doctors even use it for severe acne, post-surgical infections, and sometimes as a backup for people allergic to penicillins. One fun fact: veterinarians use it too, to treat nasty wounds or dental problems in dogs—my Max had clindamycin after a run-in with a raccoon and he bounced back like a champ. Humans usually get clindamycin as capsules, topical gels, solutions, or as an IV drip when things are bad.
If you think antibiotics are all pretty much the same, here’s something that sets clindamycin apart: it covers a mix of aerobic (oxygen-loving) and anaerobic (oxygen-hating) bacteria. That makes it a go-to for serious infections where the usual drugs—like amoxicillin—just don’t cut it. Since drug-resistant bugs are on the rise, clindamycin is often saved for cases where resistance is known or suspected.
Here’s a simple table showing what conditions clindamycin often fights, and how it’s usually taken:
| Condition | Type of Clindamycin | Route |
|---|---|---|
| Dental abscess | Capsules or liquid | Oral |
| Severe acne | Gel/lotion | Topical |
| Bone/joint infection | Injection | IV/IM |
| Post-surgical infection | Injection | IV/IM |
| Soft tissue infection | Capsules/Injection | Oral/IV |
A 2023 review in "Clinical Microbiology Reviews" put it bluntly:
"Clindamycin’s value endures because of its broad and reliable coverage against anaerobes and many Gram-positive cocci, and its continued effectiveness in penicillin-allergic patients."
So, while it’s not the first pick every time, clindamycin is far from obsolete.
Risks, Side Effects, and What Can Go Wrong
There’s no way around it—if you’re taking clindamycin, you need to watch for side effects. The most famous scare here is C. diff (Clostridioides difficile) infection. This bacteria can run wild in your gut after you wipe out the good bacteria, leading to misery-level diarrhea and even, sometimes, life-threatening colon issues. Clindamycin is one of the top culprits doctors watch for with C. diff; nobody gets this stuff without a reason.
The usual risks are these:
- Nausea and stomach pain
- Vomiting or loss of appetite
- Metallic taste in your mouth
- Throat and esophagus irritation (especially if you don’t chug enough water with the pill)
- Rash or itching—sometimes severe, as in Stevens-Johnson syndrome
- Superinfection—meaning you kill one kind of bug and another comes out to party
Doctors will warn you about diarrhea, because if you get loose stool and it smells dangerously foul, or you notice blood, you need to call immediately. It could be C. diff starting up. And don’t ignore those allergic reactions—hives, swelling, trouble breathing—as they hit faster than you might think.
You also need to know that food interacts with clindamycin absorption, but the catch is mostly about tummy comfort—if you take it with food, your gut might feel a little better, but don’t expect less risk for effectiveness. Liquid clindamycin is known for tasting absolutely disgusting; if you’re giving this to a kid, brace yourself and maybe chase it with something strong tasting.
For those allergic to penicillin, clindamycin often feels like a safe haven, but you should double check: some people are allergic to both, and that’s not the party you want to attend. As always, full and honest communication with your doctor is key.
The Smart Way to Take Clindamycin and Avoid Trouble
Even though clindamycin is tough on bacteria, you have to play by the rules or risk trouble. First off, don’t skip doses and finish the whole course—even if you feel fine halfway through. If you stop early, the strongest, ugliest bugs can come roaring back and then you’re back at square one, possibly with even less effective antibiotic options. This happens more than you’d think, especially with the pressure to avoid unnecessary antibiotics.
Doctors always repeat this but it’s worth hammering home: don’t use someone else’s clindamycin, and don’t save leftover pills to use later. The right dose and duration really are tailored to your unique infection and health story. Sharing antibiotics might sound helpful or thrifty, but it’s a recipe for drug resistance.
If you take it by mouth, wash it down with a full glass of water and try to stay upright for at least half an hour. This little habit keeps your throat and esophagus from burning—a tip that comes straight from both doctors and folks who have learned the hard way.
Be honest about your medical history. If you’ve had bowel disease, liver problems, or you’re on other antibiotics, your risk with clindamycin might be higher. Pregnant or breastfeeding? Most studies suggest the risks to your baby are low with clindamycin, but always double check with your doc before starting any new medicines (the FDA puts clindamycin in the “B” pregnancy category).
If you’re on acne gel, don’t pile it up with other drying products. Your skin can turn into a peeling fire hazard. Try to stick to gentle cleansers, avoid harsh toners or astringents, and if you’re using makeup, choose non-comedogenic products so you don’t block up your pores further.
Have pets? Clindamycin can be prescribed for them too, but always go through your vet. Doses, side effects, and monitoring rules differ from humans—and the liquid will still taste awful even to your dog like Max.
Tips and Insights for Clindamycin Users
If clindamycin comes into your life, a little preparation helps. Always ask your doctor the basics: how many days, best times for your doses, what side effects to watch for, and when to panic and call back. If you’re using topical clindamycin, wash your hands thoroughly after applying. For gels, don’t mix with heavy creams unless your skin doctor says so.
It’s smart to keep track of your symptoms while you’re on this drug. A little journal entry about how many times you have to run to the bathroom can tip you off early if something’s going wrong. Likewise, if you notice a rash or any worrisome symptoms, photos can help. Even a subtle side effect—like a weird taste—can tell your doctor something useful.
If you have a habit of probiotics, ask your doctor whether they’re safe to take with clindamycin. There’s some research out of the Mayo Clinic in 2022 suggesting specific probiotics (like Saccharomyces boulardii) may lower your risk of antibiotic-associated diarrhea, but it’s not a universal fix.
One under-rated tip: if you get a prescription for liquid clindamycin, store it in the fridge and shake it up well before pouring a dose. If the taste is too horrible, try plugging your nose as you drink or chase it with a spoonful of yogurt.
Parents, if your kid’s on clindamycin, let their teachers know. You don’t want them caught off-guard if your child runs to the bathroom or feels ill during class.
Take clindamycin seriously. It’s a heavy hitter, not just another mild-mannered antibiotic. Handle it with the respect it deserves and you’ll get your health back without too much drama—or at least avoid the worst kind of drama.





Comments (12)
Sandy Gold
Ugh, people always think antibiotics like clindamycin are some miracle cure-all, but honestly, there's so much nuance that's often skipped over. For starters, not everyone needs it, and inappropriate usage contributes to antibiotic resistance — yeah, the thing that everyone pretends is just some distant problem. Also, side effects? They're not just minor annoyances. Clindamycin can cause some serious gut problems, like C. diff infections, which are no joke. So it's really important to weigh risks before popping antibiotics like candy.
Also, let’s not ignore proper dosing. Some docs just prescribe it casually without discussing duration or potential interactions. And frankly, dental and bone infections can be tricky; sometimes this drug isn’t even the best choice. Just saying, a lot more critical thinking is needed before haphazardly using it.
Anyway, anyone else tired of the constant antibiotic hype without the full story?
Frank Pennetti
Yeah, without a doubt, clindamycin is part of a broader pharmacopeia that gets overused in the US thanks to lax prescribing standards. The rampant overprescription drives multidrug resistance and creates a public health nightmare. It's not just about personal health, folks. National healthcare policies should clamp down on misuse and incentivize narrow-spectrum agents when possible.
Plus, the jargon-heavy warnings and risks are often glossed over by both doctors and patients. You gotta understand the pharmacodynamics here, including the drug's impact on anaerobic flora and the associated risk for superinfections. Call me a nerd but these details matter.
We need more savvy patients and stricter regulation to stop this antibiotic free-for-all.
Keri Henderson
Hey everyone, I just want to emphasize how crucial it is to follow your doctor's instructions when using clindamycin. It's not just about taking the medication but completing the entire prescribed course even if you start feeling better. Incomplete courses can actually strengthen bacteria rather than eliminate them. And if you notice any severe reactions like rashes or severe diarrhea, don't hesitate to seek medical advice immediately.
Remember, this antibiotic can be life-saving when used correctly. So let's focus on education, adherence, and responsible use rather than fear or misinformation.
elvin casimir
First off, let's be clear. The post should be more meticulously proofread. Simple grammar mistakes undercut credibility when discussing antibiotics like clindamycin that demand precise communication.
That aside, I have to call out some omissions here. What about the contraindications? Patients with a history of antibiotic-associated colitis must avoid this drug. And what about its use during pregnancy or breastfeeding? These are vital details doctors and patients alike must consider.
The summary feels rushed and poorly constructed. An authoritative post requires rigor and clarity, especially in medicine where misinformation can do harm.
Steve Batancs
From a formal perspective, clindamycin is an essential option for some bacterial infections where beta-lactams aren’t viable. However, it’s crucial to remember its role as a second-line antibiotic and not a go-to for every skin, dental, or bone infection.
Risks such as Clostridioides difficile colitis are well documented and remind us of the delicate balance we must maintain in antibiotic stewardship. It serves as a reminder that antibiotics are powerful tools that require prudent application.
Overall, educational posts on this topic should stress both efficacy and risk and help foster a rational, evidence-based approach to use.
Ragha Vema
OMG, I feel like every time I hear about antibiotics, there’s this shadowy giant pharma agenda hiding behind it. Clindamycin? Sure, it works, but at what cost? What about the long-term effects on microbiomes, the stuff they never teach you, right? There’s a whole conspiracy how they push these meds and doctors just blindly follow orders, no questions asked.
And the risk of side effects? They hide that info until it’s too late! People get gut infections that ruin them for life, but that info barely sees the light of day in big advertising campaigns or patient leaflets.
Just saying, better safe than sorry, but society ignores these warnings to keep the profits rolling in!
Scott Mcquain
One must consider the ethical obligation to use clindamycin judiciously to preserve its efficacy for future generations. Using antibiotics without thorough clinical justification promotes the spread of resistant strains, which is morally untenable given the collective impact on public health.
Patients must also be counseled on the potential adverse effects and the importance of informed consent with regard to treatment risks. Precision in medical communication cannot be overstated.
The discussion surrounding this antibiotic calls for a balance between individual treatment benefits and societal responsibilities.
kuldeep singh sandhu
Well, honestly I don't see what's the big deal about clindamycin here. It’s a standard antibiotic used globally, and frankly, the complications are overstated a bit. Sure, side effects exist but so do for all drugs, right? In India, we often have to use such medicines because access to newer antibiotics is limited and cost is a factor too.
Sometimes, I wonder if some of these fears raised are just western paranoia. Not saying don’t be careful, but context matters. The basics of proper use and medical advice should still be followed.
Mariah Dietzler
Honestly, this article didn’t give me enough info. Like, what about how to handle missed doses? Or what to do if you get a mild rash — keep taking it or stop? This stuff is super common but details matter so much.
Side effects are mentioned, but no real guidance on how often they occur or what stats backs it up. Would have loved a little more depth without the scare tactics.
It’s a quick read but leaves me wanting a fair bit more. Others feel the same?
Nicola Strand
While I appreciate the effort to inform about clindamycin, I find the tone somewhat simplified and lacking in proper clinical nuance. Proper antibiotic stewardship should be highlighted more. This medication is powerful and should not be wielded lightly nor without a robust understanding of its place in therapy.
Furthermore, there's an ethical dimension to prescribing practices that goes beyond just side effects and risks. It's about preserving antibiotic utility in a world where resistance threatens to erode medical advances.
Consider this a call to elevate discourse around such treatments.
Jackie Zheng
From a linguistic and philosophical angle, the way we communicate about drugs like clindamycin shapes public perception. The casual use of phrases like "powerful antibiotic" carries connotations that may induce unnecessary fear or misplaced confidence.
Language users should strive for clarity, nuance, and honesty. Side effects and risks should be explicitly detailed to empower informed consent, not to alarm or mislead.
It's fascinating how medicine and language intertwine here, influencing how patients approach treatment and trust healthcare providers.
Keri Henderson
Adding to what was said earlier, I want to stress the importance of not self-medicating with clindamycin. Infections can appear similar but may require different treatments, so a healthcare professional's diagnosis is crucial.
And don't hesitate to discuss any other medications or supplements you're taking with your doctor or pharmacist. Drug interactions can sometimes worsen side effects or reduce efficacy.
We all share responsibility for safe antibiotic use, so passing accurate info along is key.