
Getting the right dose of medicine for a child isn’t about age. It’s not about how tall they are. It’s not even about what the bottle says for "children." It’s about their weight. And getting it wrong can be dangerous.
Every year, thousands of children in the U.S. and around the world receive incorrect doses of medication-not because doctors made a mistake, but because the math got lost in translation. A parent reads "10 mg/kg" on a prescription, doesn’t know how to convert pounds to kilograms, and guesses. A nurse calculates the dose but forgets to double-check the concentration. A pharmacist fills the prescription using an outdated formula. These aren’t rare events. They’re systemic problems-and they’re preventable.
Why Weight Matters More Than Age
Imagine two 3-year-olds. One weighs 12 kg. The other weighs 20 kg. That’s a 67% difference in body mass. If you gave both kids the same dose based on age alone, the lighter child could get too much. The heavier one might get too little. Neither outcome is safe.
That’s why weight-based dosing is the gold standard. Most pediatric medications-antibiotics, pain relievers, seizure drugs, even chemotherapy-are dosed in milligrams per kilogram (mg/kg). Some, like cancer drugs, use body surface area (BSA), but weight is the starting point for nearly all of them.
Age-based dosing? It’s outdated. It was used decades ago because scales were less common and calculations were harder. Today, we have digital scales, electronic health records, and calculators. There’s no excuse for guessing.
The Basic Math: mg/kg Explained
Let’s say your child needs amoxicillin at 25 mg/kg/day, divided into two doses. Their weight is 22 pounds.
Step 1: Convert pounds to kilograms.
22 lb ÷ 2.2 = 10 kg
That’s the rule: 1 kg = 2.2 lb. No exceptions. No rounding up. No "close enough." If you use 2.25 or 2.0, you’re already off-and that’s where errors happen.
Step 2: Multiply weight in kg by the dose.
10 kg × 25 mg/kg = 250 mg/day
Step 3: Divide by how many times per day the dose is given.
250 mg ÷ 2 = 125 mg per dose
Step 4: Convert to volume if it’s a liquid.
If the amoxicillin is 250 mg/5 mL, then:
125 mg ÷ (250 mg/5 mL) = 2.5 mL
That’s your dose. Not 3 mL. Not "a teaspoon." Exactly 2.5 mL.
It sounds simple. But in practice, mistakes happen at every step.
Where the Math Goes Wrong
The Institute for Safe Medication Practices says 80% of pediatric dosing errors involve unit conversion. That’s not a typo. That’s the main cause.
Here’s what goes wrong:
- Using pounds instead of kilograms in the calculation
- Confusing "mg/kg/day" with "mg/kg/dose"-one means total daily, the other means per administration
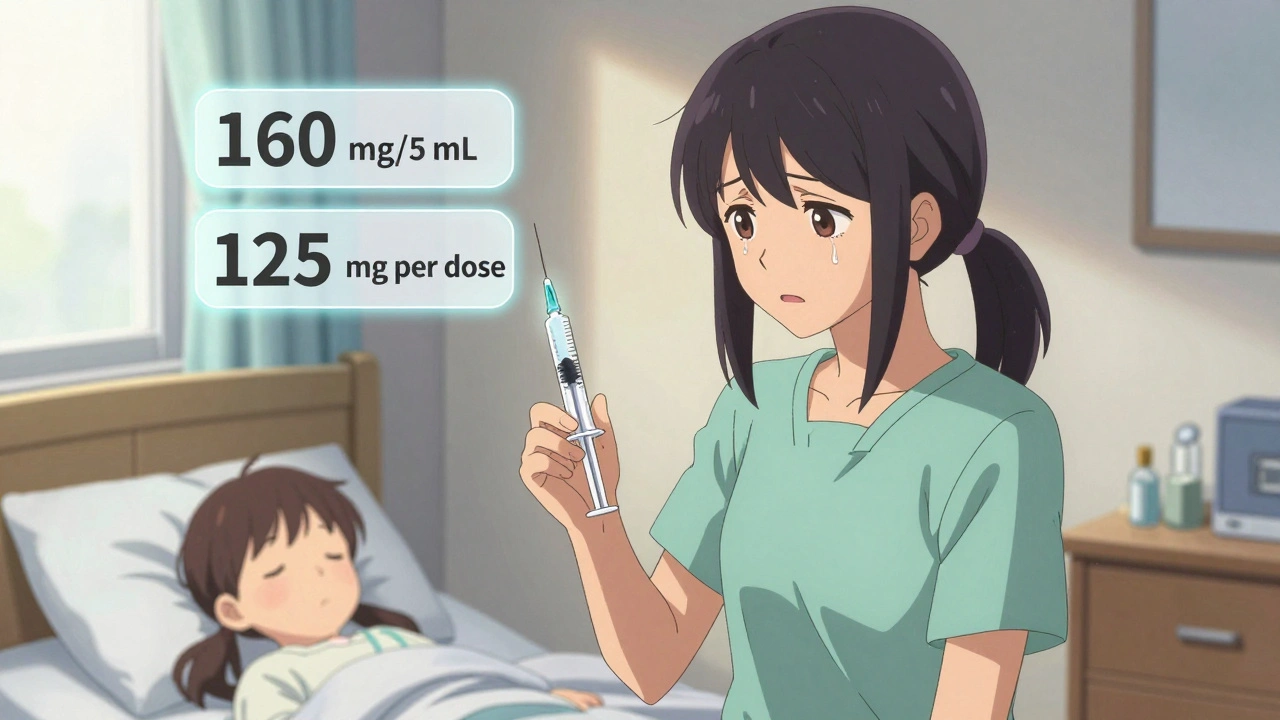
- Forgetting to convert concentration (e.g., thinking 160 mg/5 mL is the same as 500 mg/5 mL)
- Reading "mg/kg/d" as "mg/kg/day" when the prescriber meant "mg/kg/dose"
A 2021 case study in the Journal of Pediatric Pharmacology and Therapeutics reported a 15 kg child given 10 times the correct dose of amoxicillin because the nurse used the child’s weight in pounds (33 lb) and multiplied it by 25 mg/kg-instead of converting to kg first. The child ended up in the hospital with severe vomiting and dehydration.
Another common error: mixing up infant and children’s formulations. Infant acetaminophen is 160 mg/5 mL. Children’s is often 160 mg/5 mL too-but some brands use 500 mg/5 mL. One drop too many, and you’ve doubled the dose.
When Weight Isn’t Enough
Weight-based dosing works for most drugs. But not all.
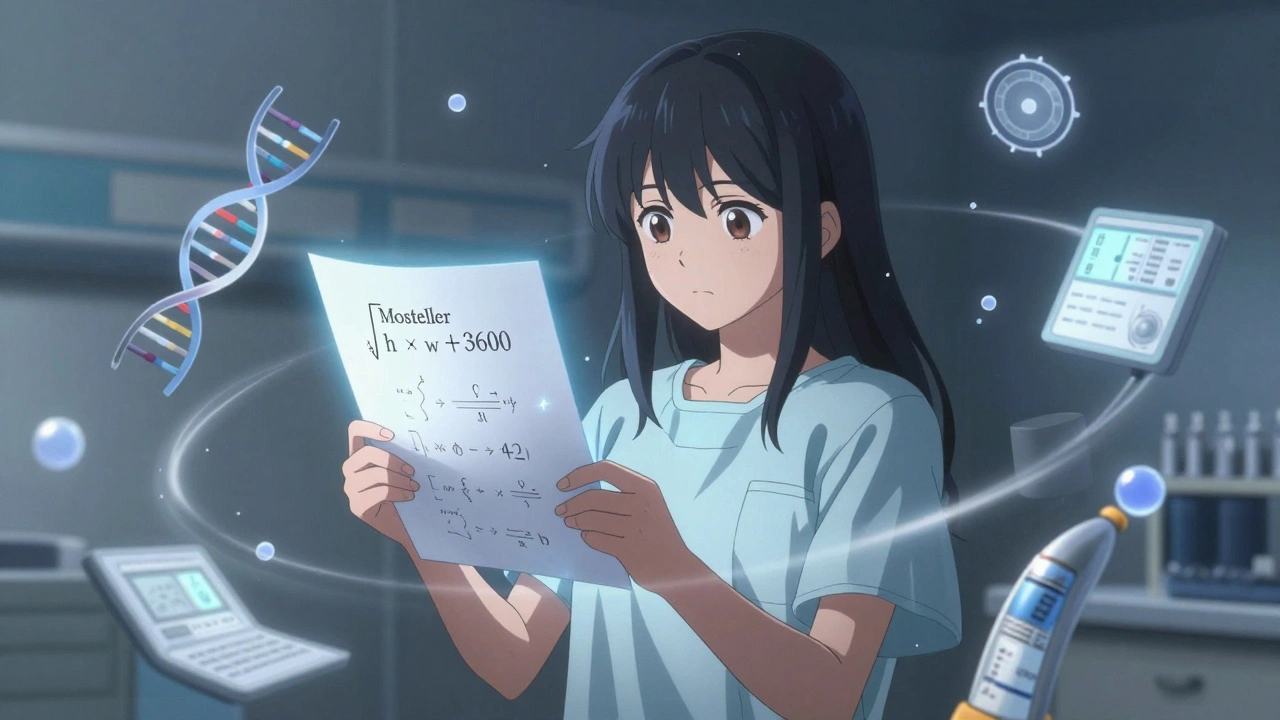
Chemotherapy drugs like vincristine use body surface area (BSA), calculated with the Mosteller formula:
BSA (m²) = √[height (cm) × weight (kg) ÷ 3600]
For a child who’s 97 cm tall and weighs 16.8 kg:
√[(97 × 16.8) ÷ 3600] = √[1629.6 ÷ 3600] = √0.4527 = 0.67 m²
The dose is then calculated as mg/m², not mg/kg. This matters because chemotherapy has a very narrow safety margin. A 10% error can be life-threatening.
Also, some drugs have weight caps. Buprenorphine, for example, is dosed by weight-but capped at 0.4 mg/kg/hour for older children, even if they weigh more. Giving more doesn’t help. It just increases risk.
And then there are age-specific warnings that override weight. Benadryl (diphenhydramine) should never be given to infants under 6 months. For children under 2 years, it’s only safe if a doctor says so. No amount of math changes that.
How Hospitals Get It Right
Hospitals don’t rely on people doing math by hand. They use systems.
- Electronic health records (EHRs) like Epic and Cerner auto-convert pounds to kilograms and calculate doses when you enter the weight.
- Dual verification: Two nurses check the calculation before giving any high-alert medication.
- Standardized order sets: Instead of writing "give 25 mg/kg," the prescriber selects a pre-built order that auto-calculates based on weight.
- Mandatory dual entry: Some systems require you to enter the weight in both pounds and kilograms. If they don’t match, the system won’t let you proceed.
A 2023 study in JAMA Pediatrics found that hospitals using these systems reduced dosing errors by 57%.
But not every parent has access to an EHR. Not every pharmacy has automated systems. That’s why knowing the basics matters-even if you’re just giving Tylenol at home.
What Parents Need to Know
If you’re giving medication to your child at home:
- Always weigh your child on a digital scale. Don’t guess. Don’t use last year’s weight.
- Convert pounds to kilograms: Divide by 2.2. Write it down.
- Read the label. Is it 160 mg/5 mL? 500 mg/5 mL? Those are completely different.
- Use the syringe that comes with the medicine. Never use a kitchen spoon.
- If the prescription says "mg/kg/d," ask the doctor: "Do you mean per day or per dose?"
- Keep a log: Write down the date, time, weight, dose given, and concentration used.
And remember: if you’re unsure, call your pediatrician. Don’t rely on internet calculators or apps that aren’t from a hospital or pharmacy. Many are outdated or inaccurate.
What’s Changing in 2025
The American Academy of Pediatrics updated its guidelines in March 2023 to require dual verification for all high-alert medications in hospitals. That’s now standard.
Electronic health record vendors are rolling out new features. Epic’s 2024 update will require weights to be entered in both pounds and kilograms. If they don’t match, the system flags it.
The Institute for Safe Medication Practices is pushing to eliminate the abbreviation "mg/kg/d" entirely. It’s too confusing. Now, they want prescribers to write either "mg/kg/day" or "mg/kg/dose." No shortcuts.
And research is moving toward personalized dosing. The NIH’s Pharmacogenomics Research Network found that genetic differences affect how 40% of children metabolize common drugs. In the future, dosing may include genetic testing-but that’s still years away. For now, weight is still king.
Final Rule: When in Doubt, Pause
Medication errors in children are almost always preventable. They happen because someone rushed. Because they assumed. Because they didn’t double-check.
The most dangerous word in pediatric dosing is "probably."
"I think the scale is right."
"This looks like the right concentration."
"They’re about 15 kg, so I’ll round up."
Stop. Pause. Verify.
Weight in kg? Check.
Dose per kg? Check.
Concentration? Check.
Double-check? Check.
It takes 30 seconds. It could save a life.
How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, if your child weighs 33 pounds, 33 ÷ 2.2 = 15 kg. Always use 2.2-never round to 2 or 2.5. This is the only conversion factor accepted in clinical practice.
What if the prescription says "mg/kg/d"?
Ask the prescriber to clarify. "mg/kg/d" is ambiguous. It could mean milligrams per kilogram per day (total daily dose) or milligrams per kilogram per dose. In practice, this confusion causes 15% of pediatric dosing errors. Always confirm whether the dose is meant to be given once a day or divided into multiple doses.
Can I use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary widely in size. A teaspoon can hold anywhere from 3 to 7 mL. Always use the syringe or dosing cup that comes with the medicine. These are calibrated for accuracy.
Why is Benadryl not recommended for young children?
Diphenhydramine (Benadryl) can cause serious side effects in children under 2, including seizures, rapid heart rate, and respiratory depression. Even if the weight-based dose seems correct, age is a contraindication. Never give it to infants under 6 months, and only use it for children under 2 if a doctor specifically says so.
Are there any medications that don’t use weight-based dosing?
Yes. Some drugs, especially chemotherapy agents like vincristine, use body surface area (BSA) instead. Others, like certain vaccines or antivirals, may use fixed doses based on age or clinical guidelines. Always check the prescribing information or ask your provider which method applies.





Comments (9)
Conor Forde
So let me get this straight - we’re now treating parents like human calculators? 🤯 Next they’ll make us balance nuclear equations before giving Tylenol. I gave my kid amoxicillin last week using a kitchen spoon because the syringe was ‘lost’ - and guess what? She didn’t die. She danced. In fact, she’s now a professional salsa dancer. Coincidence? I THINK NOT.
patrick sui
Great breakdown - especially the part about mg/kg/d being ambiguous. That’s a silent killer in clinical settings. I work in pediatrics in Dublin, and we’ve seen 3 near-misses in the last 6 months because of that exact abbreviation. The shift to writing out 'per day' or 'per dose' is long overdue. Also, dual verification isn’t just policy - it’s a moral imperative. When a kid’s life is on the line, ‘close enough’ is the enemy.
Declan O Reilly
Weight isn’t king - it’s just the best king we’ve got right now. But here’s the real question: why are we still using kg and lb in the 21st century? Metric is universal. Why do we still force American parents to divide by 2.2 like it’s some sacred ritual? We’ve got smartphones, AI, voice assistants - why isn’t every prescription auto-converted on the screen? The system is broken because we’re clinging to analog thinking in a digital age. It’s not laziness - it’s institutional inertia. And inertia kills.
Louise Girvan
This is all a lie. The FDA, WHO, and Big Pharma are pushing weight-based dosing to sell more syringes. They know parents can't do math - so they make you buy 17 different bottles. Also, digital scales are rigged. I weighed my kid twice - one said 15kg, the other said 11kg. The second one was right. The first one was planted by the pharmaceutical lobby.
soorya Raju
Bro… this whole thing is a distraction. In India, we give kids half a tablet crushed in jam because that’s what works. No scales. No apps. No ‘2.2’. We use the ‘mom test’ - if they don’t cry after, it’s fine. And guess what? Our pediatric mortality rate is lower than yours. Maybe your problem isn’t math - it’s overthinking. Let the mothers decide. They’ve been doing this for 10,000 years without a calculator.
Dennis Jesuyon Balogun
Let’s not romanticize the Western model. In Lagos, we don’t have EHRs. We don’t have dual verification. We have mothers, grandmothers, and a single vial of paracetamol with a faded label. The truth? Weight-based dosing is a luxury. But here’s what’s real: trust. When a nurse looks you in the eye and says, ‘I’ve done this 200 times,’ you believe her. Systems can fail. Human intuition - when trained - doesn’t. Maybe the answer isn’t more tech. Maybe it’s more respect for caregivers who do this without tools.
Grant Hurley
Big YASSS to the ‘pause’ rule. I once gave my 2-year-old 2.5 mL of amoxicillin thinking it was 5 mL because the syringe looked ‘about right.’ Turned out I was off by 50%. She threw up for 3 hours. Now I always double-check. And I write it down. And I take a deep breath. And I say ‘I’m not rushing’ out loud. It’s weird. But it works. Also, kitchen spoons are evil. Don’t listen to the spoon people.
Lucinda Bresnehan
As a nurse who’s seen a 14-month-old go into seizures from a 10x overdose of acetaminophen because the parent used the children’s bottle instead of the infant one - I’m begging you: please, please, please read the label. Twice. Then read it again. The difference between 160 mg/mL and 500 mg/mL isn’t a typo - it’s a funeral. And yes, I’ve had to tell a mom her baby didn’t make it because of a misplaced decimal. Don’t be that person. Pause. Verify. Call your pharmacist. They’re not judging you. They’re saving lives.
Kshitij Shah
Wow. So we’re now making parents do pharmacy school before bedtime? 😂 Meanwhile, in India, we just give the same dose as the older sibling and hope for the best. Also, ‘2.2’? Who even uses that? I divide by 2 and call it a day. My cousin’s kid took 10x the dose and now he’s a chess champion. Coincidence? I think not. Also, Benadryl? My grandma used it to make toddlers sleep on long bus rides. She’s 92. Still alive. So… maybe we’re overcomplicating this?