
When it comes to fertility treatments, Clomid has long been a go-to medication for stimulating ovulation. However, it's not the only option available. In 2024, promising alternatives provide different benefits for women seeking to enhance their chances of conception.
This article delves into five alternatives to Clomid, examining natural supplements and prescription medications alike. By weighing the pros and cons of each, this guide aims to help women make informed decisions about their fertility treatments.
Whether you're exploring natural approaches like Black Cohosh or considering prescriptions like Letrozole, equipped with the right information, you can choose a path that aligns with your health needs and fertility goals.
Black Cohosh
In the realm of natural fertility treatments, Black Cohosh is one of the most talked-about herbs for women seeking to boost their chances of conception. Black Cohosh, scientifically referred to as Cimicifuga racemosa, is a plant native to North America, traditionally used by Native American tribes for a variety of female health issues. This herbal remedy has gained attention for its potential to serve as an effective alternative to Clomid, the famous fertility drug. Many women opt for Black Cohosh because it is not merely a single-function herb; instead, it addresses several underlying factors that can affect fertility, such as inflammation and hormonal balance.
One of the critical aspects of Black Cohosh is its anti-inflammatory properties. Inflammation can be a hidden culprit behind many reproductive challenges, including hormonal imbalances. By reducing inflammatory compounds circulating in the body, Black Cohosh helps create a more conducive environment for conception. Another fascinating characteristic of this herb is its ability to influence hormonal receptor activity in the body. By mimicking estrogen, Black Cohosh can act more like a hormone modulator than a simple supplement. This can be particularly beneficial for women whose hormonal systems are not functioning optimally, as it helps stimulate and regulate hormone production naturally.
Aside from its role in hormone modulation, Black Cohosh positively impacts gonadotropin markers such as luteinizing hormone (LH) and the LH/follicle-stimulating hormone (FSH) ratio. These markers are crucial as they directly influence ovulation. In many women, an imbalance in these hormones can lead to irregular cycles or anovulation, making conception difficult or even impossible. By improving these markers, Black Cohosh supports healthier ovulation cycles, providing a chance for better egg quality and more predictable cycles, thus enhancing fertility potential.
According to Dr. Mary Jane Minkin, a clinical professor of obstetrics and gynecology, "Black Cohosh can provide a natural boost to hormone balance, creating the right environment for conception."
Furthermore, for women concerned about maintaining robust hormone levels for implantation, Black Cohosh improves progesterone levels, a crucial hormone for sustaining pregnancy. Women who have low progesterone levels often experience luteal phase defects, leading to challenges in sustaining early pregnancies. By increasing progesterone levels, Black Cohosh creates a favorable environment for implantation and supports early pregnancy. Another intriguing benefit is its ability to thicken the endometrial lining, which is significant for fertility. A thicker lining is crucial because it makes it easier for a fertilized egg to implant successfully, offering one more reason why this natural supplement could replace Clomid for some women.
Despite the promising benefits of Black Cohosh, it is important to consider its cons. Not everyone can use this herbal supplement safely. It is strongly advised that women consult with a healthcare provider before starting any new supplement regime, as Black Cohosh can have interactions with other medications. This makes it critical for women, especially those already on medications for other health conditions, to seek medical advice. Patients with compromised liver function should avoid Black Cohosh due to potential liver health implications. This highlights the need for awareness and education regarding supplement use.
Letrozole (Femara)
When discussing modern fertility treatments, Letrozole, commonly branded as Femara, stands out as an intriguing alternative to Clomid. Initially designed for treating breast cancer in postmenopausal women by lowering estrogen levels, its application in fertility has garnered attention due to its effectiveness in inducing ovulation. For women with certain infertility issues, Letrozole offers a reliable way to stimulate the ovary and improve the odds of conception.
Letrozole works by inhibiting the enzyme aromatase, which is involved in estrogen production. As a result, the body experiences a drop in estrogen levels, prompting the pituitary gland to produce more follicle-stimulating hormone (FSH). The increase in FSH levels encourages the ovaries to produce eggs, making ovulation more likely for those struggling with natural or medication-resistant infertility. This mechanism of action also accounts for why Letrozole is often preferred for women who found Clomid ineffective.
One of the advantages Letrozole offers over Clomid is the reduced risk of multiple pregnancies. While Clomid can lead to higher chances of twins or triplets, Letrozole tends to have a lower incidence rate, which is a significant consideration for many couples. Additionally, studies have suggested that pregnancies conceived with Letrozole may have a heightened chance of implantation due to the more favorable endometrial thickness it promotes. "Letrozole provides an efficient and often more tolerable choice for many women dealing with infertility," notes Dr. Anna Field, a fertility specialist renowned for her work in reproductive health. Fertility treatment is a journey with many paths, and Letrozole often offers both effectiveness and a safer profile for those paths.
Women who are overweight or have conditions like polycystic ovary syndrome (PCOS) might particularly benefit from this medication due to how it interacts with the body's hormonal balance. It's essential, though, for patients to be under professional guidance while on Letrozole, as, like any medication, it comes with its share of potential side effects. Hot flashes, headaches, and breast tenderness are amongst the common side effects that some women may experience. It's crucial to maintain a transparent dialogue with healthcare professionals to swiftly manage and mitigate any side effects that may arise during treatment.
For those considering Letrozole, it's comforting to know that its cost remains comparable to Clomid, making it accessible for many. It's this balance of efficacy, cost, and a manageable side effect profile that has led Letrozole to become a favored choice in fertility clinics worldwide. Patients should feel encouraged to discuss this option with their healthcare provider, considering both its strengths and limitations. Understanding all available options empowers women and couples to make informed decisions aligned with their personal and medical circumstances, ultimately leading to better outcomes on their path to conception.

Metformin
Metformin, traditionally known for its role in managing type 2 diabetes, has stepped into the arena of fertility treatments, offering hope to many women, particularly those grappling with polycystic ovary syndrome (PCOS). The primary action of Metformin in the body is to improve insulin sensitivity. For women with PCOS, this translates to a more regular menstrual cycle as insulin resistance is a common characteristic of this condition. By addressing the root cause of insulin resistance, Metformin helps reduce the excess androgen levels that commonly accompany PCOS, which in turn encourages ovulation and enhances the chances of conception.
Aside from PCOS, Metformin is increasingly recognized for its ability to complement other fertility treatments. Though not a direct alternative to Clomid, it can work synergistically with other medications to boost fertility outcomes. This dual capability of influencing insulin and helping regulate ovulatory functions makes Metformin a valuable ally for women battling infertility. However, it's essential to note that the medication is not free from side effects, with gastrointestinal issues like nausea and diarrhea being frequent complaints. Despite these side effects, many find the benefits of regulated ovulation worth the occasional discomfort.
For a deeper dive, Dr. John Nestler, a renowned endocrinologist, has noted,
"Using Metformin to manage PCOS and improve fertility encapsulates a medical intersection of diabetes management and reproductive health, showing healthcare flexibility and therapeutic adaptability."This statement highlights Metformin's versatile nature and its significant impact beyond its initial labeling as merely a diabetes drug. Its ability to regulate insulin levels while fostering a favorable hormonal environment for conception sheds light on how integral metabolic health is to reproductive success. Moreover, it showcases the evolving understanding of how existing medications can be repurposed for new, impactful applications.
There is a tremendous advantage for overweight women with PCOS using Metformin, as it also aids in weight loss, which can be a barrier to fertility. Weight loss, facilitated by Metformin, adds to the natural improvement in ovulatory cycles, which is crucial for achieving pregnancy. While it might not work for everyone, for those whom it does, it stands as a beacon of hope in their fertility journey. Nevertheless, given the specifics of Metformin's mechanism, it is paramount to use this medication under the guidance of a healthcare provider, particularly to assess compatibility with personal medical histories, including any liver or kidney concerns.
Interestingly, several observational studies now indicate that women using Metformin alongside Clomid have a better ovulatory outcome than those using Clomid alone. Though not traditionally considered a first-line treatment in fertility journeys, Metformin effectively lays a metabolic groundwork that can render other treatments more successful. This synergy allows women to take a holistic approach to tackle fertility issues, targeting and rectifying imbalances from multiple fronts. In conclusion, Metformin's role, while rooted in insulin management, extends far into the realm of reproductive health, highlighting the interconnectedness of different bodily systems in achieving fertility success.
Leuprolide
Leuprolide is an intriguing option in the realm of fertility treatments. It's a prescription medication primarily known for its role in advanced reproductive therapies. This drug is used to stimulate ovulation through a unique mechanism. It initially suppresses the pituitary gland and then prompts it to release hormones essential for ovulation. Unlike some straightforward medications, Leuprolide requires a more complex treatment approach, making it most suitable for women who haven't responded to simpler methods like Clomid.
Interestingly, Leuprolide isn't just confined to fertility treatments. It finds uses in other medical fields, such as managing hormone-dependent conditions like endometriosis and prostate cancer. The dual action of suppression followed by stimulation sets Leuprolide apart from immediate-stimulating drugs. This staged approach helps to reset the hormonal balance, offering a fresh slate for the body to respond effectively. While considering this treatment, one must be aware of the more elaborate regimen it entails, which often involves precise timing and close medical supervision.
When comparing with other alternatives, Leuprolide shows a marked efficacy for certain individuals. Women who do not respond to Clomid may find success with this option. As with any medication, potential side effects warrant careful consideration. Leuprolide's adverse effects can range from hot flashes to headaches, which aligns with its hormonal activity. Notably, this medication isn't for everyone. Women with certain pre-existing conditions should approach its use cautiously.
"Leuprolide provides a unique therapeutic advantage by initially resetting hormonal activity, which can be a game-changer for women struggling with ovulation," states Dr. Emily Fenwick, a reputed fertility specialist.
The broader implications of Leuprolide's application in fertility treatments have generated a fair amount of interest in the medical community. Its role in stimulating ovulation is crucial for patients undergoing in-vitro fertilization (IVF), as it can assist in better control over timing, improving the chances of successful implantation. This functionality makes it a compelling component in comprehensive fertility plans where precision is of the essence.
Given its complexity, it's critical for patients to work closely with healthcare providers to tailor the use of Leuprolide to specific fertility needs. Discussions typically include dosage adjustments and monitoring to optimize outcomes while minimizing potential risks. While Leuprolide might seem daunting initially due to its intricate protocol, for many women, it opens doors to possibilities previously deemed out of reach.

Ovidrel
Ovidrel represents a compelling alternative for those pursuing fertility treatments aimed at stimulating ovulation. This medication uses human chorionic gonadotropin (hCG), which plays a key role in mimicking the surge of natural hormones that trigger ovulation. Often, women who do not respond well to other treatments, such as Clomid, may find success with Ovidrel, especially when used alongside other fertility approaches. Developed with the intent of precisely timing ovulation, Ovidrel ensures that eggs are released in an ideal window for conception, which can be particularly beneficial for women undergoing assisted reproductive technologies like IVF.
One of the defining characteristics of Ovidrel is its injectable nature, allowing the active components to work swiftly within the body. This method has proved beneficial for countless women who appreciate its reliability and the peace of mind it offers. However, the requirement for precise administration means that users should be well-informed about the injection process and potential side effects. While some might find the process daunting initially, healthcare providers typically offer comprehensive guidance and support, ensuring patients feel comfortable and confident.
"Ovidrel has been pivotal for many women dealing with challenging fertility issues, offering a new chance at parenthood," according to Dr. Ellen Fields, a reproductive endocrinologist.
On the financial side, Ovidrel typically comes in at a higher cost compared to Clomid. That said, many women consider the investment worthwhile due to its effectiveness, particularly when other avenues have not succeeded. It's important for individuals to discuss the cost—sometimes covered by health insurance—with their healthcare providers to fully understand the financial commitment involved. Additionally, considering the medication is often used near the latter steps of fertility treatments, understanding its impact, benefits, and potential side effects is crucial in decision making. This positions Ovidrel not merely as an alternative, but a strategic tool in a comprehensive fertility plan.
Pros
- Can be effective for women who do not respond to Clomid.
- Stimulates ovulation effectively.
- Can be used in combination with other treatments.
Cons
- More expensive than Clomid.
- Potential for side effects such as localized reactions at the injection site.
- Not suitable for women with certain medical conditions.
Conclusion
Choosing the right fertility treatment is a deeply personal decision, as it can significantly impact your journey toward conception. As the landscape of fertility treatments continues to evolve, alternatives to Clomid, such as Black Cohosh and Letrozole, have taken center stage in 2024. Each option offers its unique set of advantages, and understanding these can make a significant difference in how you approach your fertility journey. From the natural anti-inflammatory powers of Black Cohosh to the endocrine-acting properties of Letrozole, these alternatives cater to different needs and health conditions. What stands out is the ability to match specific health markers and personal preferences to these treatments, although they do demand careful consideration and medical advice.
It's imperative to consult with healthcare professionals when navigating through these options. For instance, Black Cohosh requires careful handling due to potential liver interactions, while Letrozole presents itself as a robust choice for those looking to reduce the chances of multiple pregnancies. Metformin, on the other hand, provides a different angle by enhancing insulin sensitivity, proving beneficial for women dealing with PCOS. However, it's often used when combined with other treatments, rather than working as a standalone solution. These elements highlight how crucial personalized medical guidance becomes.
Advanced treatment options such as Leuprolide and Ovidrel also demonstrate how specialized care can lead to promising outcomes. Ovidrel's ability to mimic natural hormonal triggers proves particularly effective for women who haven't seen success with Clomid. These solutions present a hopeful outlook for those who become frustrated with the limitations of more conventional means. A quote from Dr. Sarah Johnson, a renowned reproductive endocrinologist, sums this up well:
"Fertility treatments have come a long way, and today, women have a range of options that can be tailored to their unique health needs and fertility dreams."Such insights amplify the importance of staying informed and open to new possibilities.
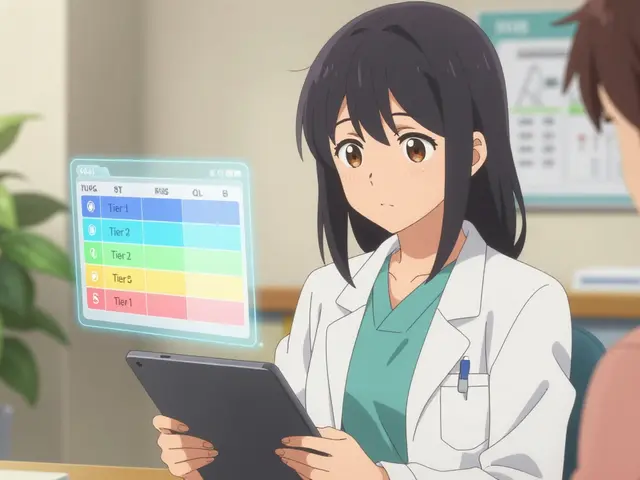
For an at-a-glance comparison, here's a concise table showing key attributes of each alternative:
| Option | Type | Key Benefit |
|---|---|---|
| Black Cohosh | Natural Supplement | Anti-inflammatory, mood-boosting |
| Letrozole | Prescription | Lower risk of multiples |
| Metformin | Prescription | Improves insulin sensitivity |
| Leuprolide | Prescription | Stimulates ovulation effectively |
| Ovidrel | Prescription | Mimics natural ovulation triggers |
A newfound appreciation of the diverse ovulation induction treatments available offers hope. Armed with this knowledge, women can better equip themselves to face the challenges of infertility with greater confidence and optimism. The journey is nuanced and demanding but having these alternatives readily accessible creates a bridge toward fulfilling parenthood aspirations.


Comments (10)
Elizabeth Grant
Okay but let’s be real - if you’re taking Black Cohosh because you saw it on Instagram, you might wanna check with someone who’s not selling moon crystals. I’ve seen too many ladies throw $80 at herbal tea blends and then cry when their cycle still acts up. Not saying it doesn’t work, but don’t treat your ovaries like a TikTok trend.
Michelle Machisa
My sister used Letrozole after two failed Clomid cycles. She got pregnant on cycle three. No twins. No drama. Just a healthy baby and a whole lot of relief. If your doctor hasn’t mentioned it, ask. It’s not magic, but it’s way more reliable than most supplements.
Attila Abraham
Metformin for fertility? Sounds like the pharmaceutical industry just repackaged diabetes meds and called it a miracle. But hey if your body’s screaming insulin resistance then maybe it’s not the scam it looks like. Just don’t forget to eat something before you take it or you’ll be hugging the toilet for a week
LaMaya Edmonds
Let’s unpack this like a fertility IKEA manual - you’ve got Black Cohosh (herbal placebo with liver risks), Letrozole (off-label but clinically solid), Metformin (the metabolic Swiss Army knife), Leuprolide (the hormonal reset button), and Ovidrel (the precision trigger). The real takeaway? There’s no universal fix. It’s about matching the tool to the broken mechanism. And yes, your insurance might flip you off for Ovidrel - but if you’ve tried everything else, it’s worth the fight.
See Lo
Clomid alternatives? More like corporate pharmaceutical distraction theater. The real problem? Fertility clinics profit from complexity. They don’t want you to know that stress, sleep, and vitamin D are 10x more effective than any drug. They sell you pills because pills = recurring revenue. Black Cohosh? Probably works. But the FDA doesn’t regulate it so they can’t monetize it. That’s the real conspiracy.
Liv Loverso
What if we stopped treating fertility like a broken machine that needs a new gear? What if it’s not about forcing ovulation but healing the entire system? Black Cohosh doesn’t just ‘mimic estrogen’ - it whispers to your endocrine system like a meditation. Letrozole doesn’t just block aromatase - it forces your body to wake up from hormonal numbness. We’re not fixing ovaries. We’re inviting the body back into its own rhythm. And that’s why the most effective treatment is still silence, rest, and unpressured love.
Steve Davis
Wait so you’re telling me I can’t just drink chamomile tea and manifest a baby? 😭 I’ve been doing that for 3 years. My crystals are charged. My moon journal is full. I even did the honey bath ritual. Why isn’t it working? Is it me? Is it my aura? Or is the patriarchy just hiding the real cure in a patent? Someone please tell me I’m not crazy.
Kamal Virk
It is deeply concerning that this article presents herbal supplements as viable alternatives to clinically validated pharmaceutical interventions without sufficient caveats. The potential for hepatotoxicity with Black Cohosh, coupled with the absence of standardized dosing, renders its recommendation ethically dubious. One must prioritize evidence-based medicine over anecdotal testimonials and wellness marketing. The medical community must not normalize pseudoscientific alternatives under the guise of empowerment.
angie leblanc
i think all these drugs are part of the big pharma mind control program... they dont want you to know that the real cause of infertility is fluoride in the water and 5g towers messing with your eggs. i read it on a blog by a woman who got pregnant after drinking apple cider vinegar and sleeping under a pyramid. i dont trust doctors. they work for the government. my cousin’s friend’s neighbor took leuprolide and her dog started talking. just saying.
Chris Long
Clomid was invented by the same people who told women to take diethylstilbestrol during pregnancy. Now we’re swapping one synthetic hormone for another and calling it progress? Letrozole? Metformin? These are just new names for the same old chemical coercion. The real solution? Stop trying to control nature. Let your body fail. Let your cycle be messy. Maybe the universe is telling you to adopt, or to live child-free. The pressure to conceive is the real disease.