
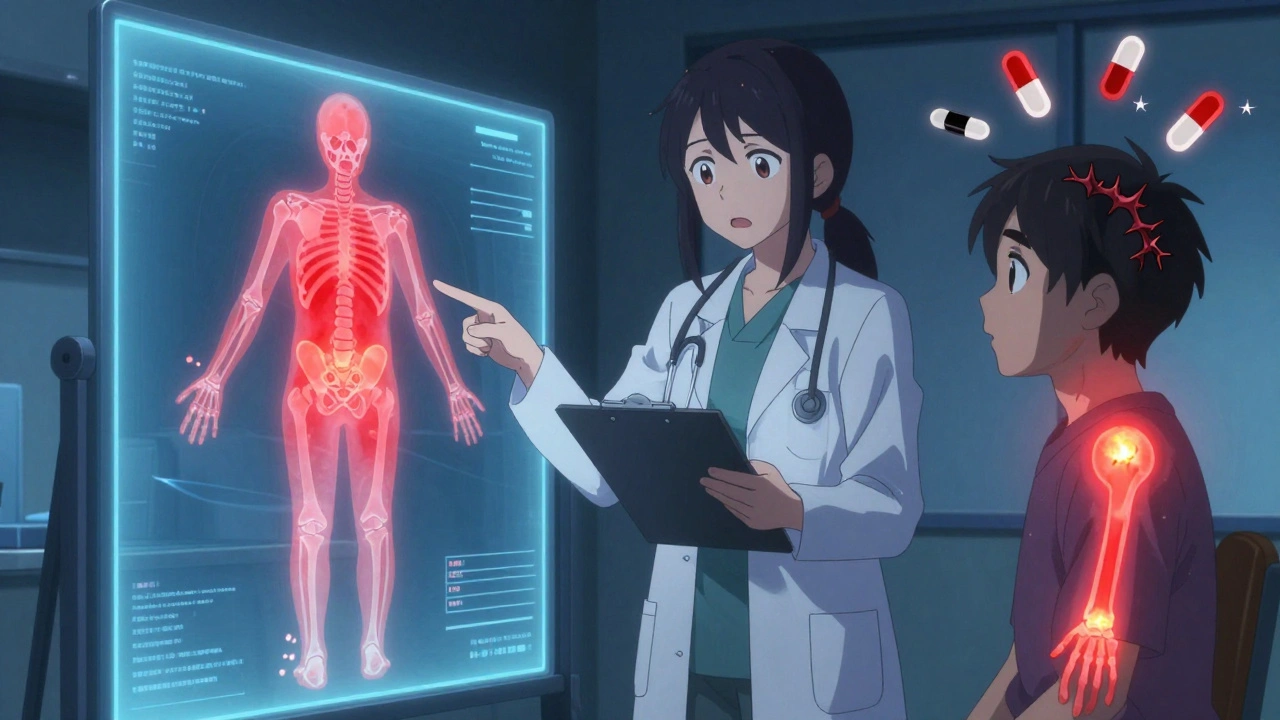
Imagine you’ve been on opioids for months to manage chronic back pain. Your dose keeps going up, but the pain isn’t just staying the same-it’s spreading. Now your legs ache, your skin hurts when you brush against your clothes, and nothing seems to help. You and your doctor might assume you’ve built up a tolerance. But what if it’s something else entirely? Something that makes opioids increase your pain instead of reducing it?
This isn’t rare. It’s called opioid-induced hyperalgesia (OIH). And it’s often mistaken for tolerance. The two sound similar-both involve needing higher doses-but they’re completely different in cause, pattern, and treatment. Getting them mixed up doesn’t just waste time. It can make pain worse.
What Is Opioid-Induced Hyperalgesia?
Opioid-induced hyperalgesia is when long-term opioid use makes your nervous system more sensitive to pain. It’s a paradox: the drug meant to dull pain ends up amplifying it. You might feel the same original pain more intensely, or you might develop new types of pain-like allodynia, where light touch feels sharp or burning.
It’s not a myth. Lab studies show it clearly. When animals are given chronic opioids, their pain thresholds drop. Human studies are harder because pain is subjective, but clinical reports confirm it. Patients on stable, high-dose opioids report worsening pain-not because their condition is progressing, but because their nerves are rewired.
Think of it like turning up the volume on a broken speaker. The signal (opioid) isn’t working right. Instead of quieting the noise, it’s making the static louder.
What Is Opioid Tolerance?
Tolerance is simpler. It’s when your body gets used to the drug. Over time, the same dose doesn’t block pain as well. You need more to get the same relief. This happens with all opioid effects-pain relief, sedation, even nausea. It’s predictable. It follows a pattern. And it’s reversible.
Unlike OIH, tolerance doesn’t create new pain. It just makes the old pain harder to control. Your pain stays in the same place. It doesn’t spread. It doesn’t change quality. You don’t suddenly feel pain from a light blanket. You just feel your original pain more.
Tolerance is why doctors sometimes increase doses. It’s expected. It’s part of the calculus. But if you’re increasing doses and pain is getting worse, that’s a red flag.
Key Differences Between OIH and Tolerance
Here’s how to tell them apart-right at the bedside.
- Pain pattern: With tolerance, pain stays where it was. With OIH, it spreads. A low back pain might start radiating down both legs, or new pain appears in the hands or feet.
- Pain quality: Tolerance doesn’t change the type of pain. OIH can bring in new sensations: burning, tingling, electric shocks, or pain from light touch.
- Response to higher doses: In tolerance, more opioid = better pain control. In OIH, more opioid = worse pain. This is the biggest clue.
- Timing: Tolerance builds gradually over weeks or months. OIH can appear suddenly after a dose increase, or even while doses are stable.
- Withdrawal vs. stable dosing: If pain spikes when you reduce the dose, it’s likely withdrawal. If pain spikes while you’re on the same dose, it’s more likely OIH.
One patient I saw had been on oxycodone for two years for degenerative disc disease. Her pain was localized to her lower back. After a dose increase, she started feeling sharp pain in her calves and couldn’t wear socks without discomfort. She wasn’t withdrawing. She wasn’t getting worse from her spine. She had allodynia-classic OIH.
How to Diagnose OIH in Practice
There’s no blood test. No scan. No single tool that says “yes, this is OIH.” But you can build a strong case with careful observation.
Start with a pain map. Ask the patient to draw where they hurt. Do it at every visit. If the area keeps growing, that’s a major red flag. Use simple tools: a 0-10 pain scale, but also ask, “Has the pain changed in how it feels?” and “Is there anything that didn’t hurt before, now hurting?”
Track dose changes. Did the pain get worse after the last increase? Did it improve when you lowered the dose-even temporarily? If yes, OIH is likely.
Look for signs of central sensitization: pain that moves, pain from touch, pain that lingers after the trigger is gone. These aren’t signs of nerve damage. They’re signs your spinal cord and brain have become hypersensitive.
Don’t rely on patient reports alone. Use standardized tools like the PainDETECT questionnaire or the DN4 tool for neuropathic pain. They’re not perfect, but they help spot patterns.
Why This Mistake Happens So Often
Doctors are trained to escalate opioids when pain worsens. That’s the default script. It’s what guidelines used to say. It’s what patients expect. And OIH is still poorly taught.
In New Zealand, opioid prescribing dropped 17% between 2018 and 2021-not because fewer people were in pain, but because clinicians started asking: “Is this really tolerance? Or is this OIH?”
Regulators like Medsafe and the FDA now warn that opioids aren’t recommended for long-term non-cancer pain. Partly because of OIH. Partly because of addiction. But also because, for many, the risks outweigh the benefits.
The problem is: if you don’t know OIH exists, you’ll keep giving more opioids. And the pain keeps getting worse. It becomes a vicious cycle.
What to Do When You Suspect OIH
Stop escalating. That’s step one.
Step two: consider a slow taper. Not cold turkey. But reduce the dose by 10-20% every week or two. Many patients report improvement within days. Pain starts to settle. The spreading stops. The allodynia fades.
Step three: switch opioids. Some opioids, like methadone or buprenorphine, have different effects on NMDA receptors-the brain pathway thought to drive OIH. Switching can reset sensitivity.
Step four: add non-opioid support. Low-dose ketamine, gabapentin, or nortriptyline can help calm overactive nerves. Physical therapy, mindfulness, and graded movement are just as important. They don’t just distract from pain-they retrain the nervous system.
One study showed that patients with suspected OIH who underwent a slow taper and started gabapentin had a 60% reduction in pain scores over 12 weeks. Those who kept increasing opioids? No improvement.
When OIH Isn’t the Problem
Not every worsening pain is OIH. Maybe the arthritis is getting worse. Maybe a new herniated disc appeared. Maybe depression is amplifying pain signals. Always rule out new pathology first.
But if imaging is normal, if pain keeps spreading, and if higher doses make it worse-OIH should be on your shortlist.
And if you’re unsure? Try a short trial of dose reduction. If pain improves, you’ve found your answer. If it gets worse, you’ve ruled out OIH and can safely explore other causes.
The Bigger Picture
Opioids aren’t the villain. For acute pain, cancer pain, or end-of-life care, they’re lifesavers. But for chronic non-cancer pain? The evidence is clear: long-term use often does more harm than good.
OIH is one of the reasons why. It’s not rare. It’s not theoretical. It’s happening in clinics right now-especially in patients on high doses for years.
What we need now isn’t more opioids. It’s better recognition. Better tools. Better training. And the courage to step back when the treatment is making things worse.
For patients stuck in this cycle, the good news is: OIH is often reversible. Not always. But often. And the sooner you recognize it, the faster they can get back to living without being controlled by a drug that’s hurting them.
Can opioid tolerance turn into opioid hyperalgesia?
Yes, they can coexist. Tolerance means you need more drug for the same effect. OIH means the drug is making your pain worse. Many patients on long-term opioids develop both. That’s why simply increasing the dose often backfires-it worsens the hyperalgesia while only temporarily masking the tolerance. The key is to treat both by reducing dose and switching medications, not just pushing higher.
Is opioid hyperalgesia the same as addiction?
No. Addiction involves compulsive use despite harm, cravings, and loss of control. OIH is a physiological change in pain processing. A patient can have OIH without being addicted. They might be taking their meds exactly as prescribed and still develop worsening pain. Confusing the two leads to stigma and poor care. You can treat OIH without assuming addiction.
How long does it take for opioid hyperalgesia to develop?
It varies. Some patients show signs after just a few weeks on high doses. Others take months or years. It depends on genetics, the type of opioid, the dose, and the individual’s pain condition. There’s no fixed timeline, but the risk increases with higher daily doses and longer duration of use.
Can you test for opioid hyperalgesia?
There’s no single lab test, but clinicians use quantitative sensory testing (QST) to measure pain thresholds. For example, they might use a pressure device or heat probe to see how much stimulus it takes to cause pain. If thresholds drop over time on opioids, it suggests hyperalgesia. Pain mapping and detailed symptom tracking are just as important in real-world settings.
What medications help with opioid hyperalgesia?
Low-dose ketamine, naltrexone, gabapentin, pregabalin, and certain antidepressants like amitriptyline or nortriptyline can help calm overactive nerves. Some doctors use buprenorphine or methadone for opioid rotation because they affect NMDA receptors differently than morphine or oxycodone. The goal isn’t to replace one opioid with another-it’s to reduce overall opioid burden and support nervous system recovery.
What Comes Next?
If you’re managing chronic pain with opioids and things aren’t getting better-stop assuming it’s tolerance. Ask: Is the pain spreading? Is it changing? Is it worse after a dose increase?
If the answer is yes, it’s time to rethink the plan. Reduce the dose. Consider alternatives. Involve a pain specialist. Don’t wait for the pain to get worse. Opioid hyperalgesia is treatable. But only if you recognize it early.





Comments (10)
Sean McCarthy
If your pain gets worse when you increase the dose you're probably dealing with OIH. Stop doubling down on opioids and start thinking about tapering.
Jaswinder Singh
Bro this is exactly what happened to my uncle. Doctor kept upping his oxycodone until he couldn't even sit on a couch without screaming. Then they finally cut the dose and he cried because it felt better. No one told him this was a thing.
Bee Floyd
I've seen this play out in chronic pain clinics more times than I can count. The real tragedy isn't the pain-it's how often the solution becomes the problem. Opioids aren't evil, but they're not magic either. Sometimes the bravest thing a clinician can do is say 'let's try less.'
Jeremy Butler
The ontological paradox of opioid-induced hyperalgesia is not merely a pharmacological anomaly, but rather a profound epistemological failure within contemporary pain management paradigms. The very mechanism intended to ameliorate suffering inadvertently engenders a pathological amplification of nociceptive signaling, thereby subverting the therapeutic intent.
Courtney Co
I just had to tell someone this story-I was on 120mg oxycodone a day for three years and my skin felt like it was on fire from my socks. My doctor said I was 'being dramatic.' I cried in the parking lot. I felt so alone. Then a pain specialist said, 'This isn't you. This is the drug.' And I finally felt seen. Please, if you're reading this and you're in pain and it's getting worse-don't blame yourself. It's not your fault.
Shashank Vira
Ah, the tragicomic ballet of modern medicine: the physician, armed with outdated protocols, administering the very toxin that mutates the patient’s nervous system into a symphony of suffering. One must ask-does the system heal, or merely ritualize its own failure?
Eric Vlach
I work in primary care and this is the most under-taught thing in med school. We get trained to titrate up when pain doesn't improve. No one tells us to look for allodynia or spreading pain. I had a patient who improved in days after cutting her dose by 30%. She didn't even know this was a thing. We need to fix this.
Souvik Datta
This is one of those moments where medicine has to grow up. We've spent decades treating pain like a simple dial you turn up. But the nervous system isn't a faucet-it's a living, breathing, sensitive network. OIH isn't a failure of the patient. It's a failure of our thinking. The good news? The body can heal. We just have to stop pushing the button that breaks it. Taper slowly. Try gabapentin. Move gently. Be patient. You're not broken. You're just overstimulated. And that's fixable.
Irving Steinberg
bro i had this exact thing and now i just do yoga and drink green tea and my back feels fine lol 😌
Matt Dean
If you're still on opioids for chronic pain you're doing it wrong. This isn't rocket science. The system is broken and you're just another statistic. Get off them. Find a real pain specialist. Stop being lazy. Your life is not a prescription pad.