
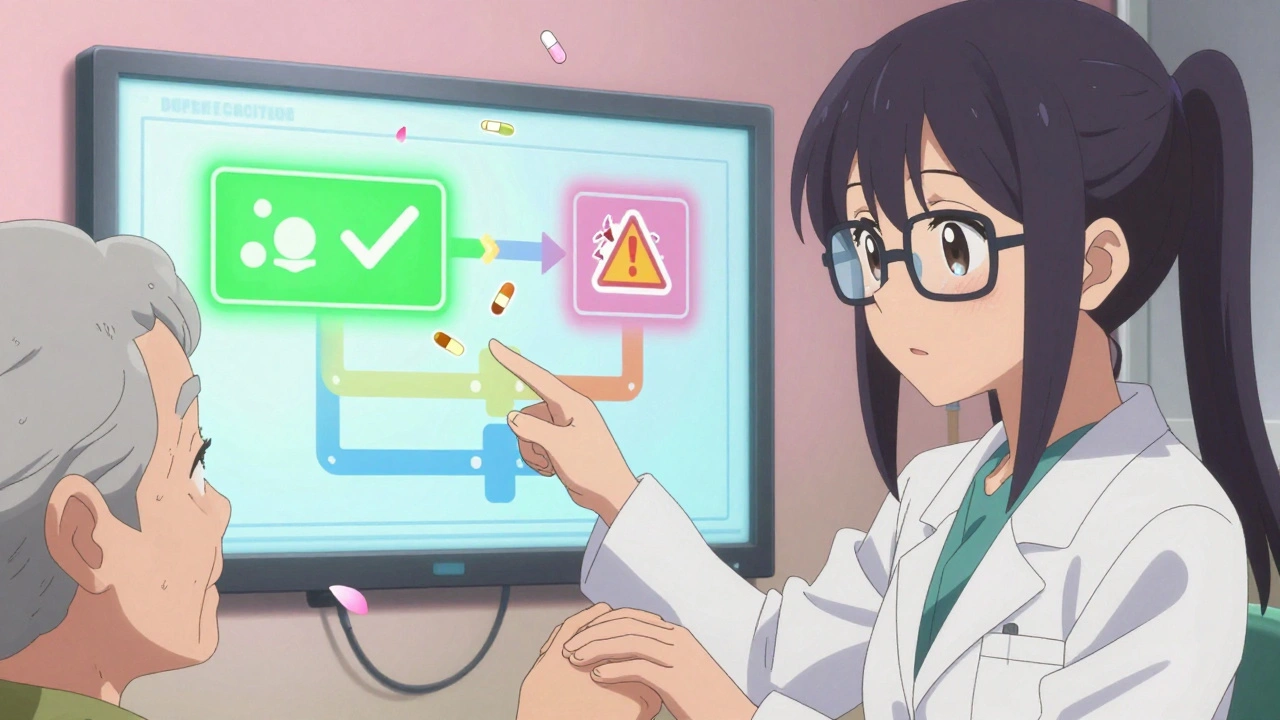
What pharmacist-led substitution programs actually do
When you’re discharged from the hospital, you might walk out with a new stack of pills - some you’ve never taken before, others you stopped months ago. That’s where pharmacist-led substitution programs step in. These aren’t just about swapping one drug for another. They’re about fixing broken medication lists before they hurt someone. Pharmacists review every pill a patient is taking, compare it to what the doctor ordered, and catch the mismatches. Maybe the patient was on warfarin at home but got started on rivaroxaban in the ER. Maybe they’re still getting a muscle relaxant they stopped six months ago. These aren’t small errors. They cause real harm.
According to data from the American Society of Health-System Pharmacists, these programs cut adverse drug events by nearly half. That’s not a guess. It’s from multi-center studies tracking real patients. In one hospital system, 3.7 medication errors were found per patient during reconciliation. That’s more than three chances per person for something to go wrong. Pharmacists don’t just spot these - they fix them. And they don’t wait for the patient to complain. They act before discharge.
How these programs are built - step by step
There’s no single way to run this, but the best programs follow a clear structure. It starts with trained medication history technicians. These aren’t just clerks. They’re the frontline. They interview patients, check old pharmacy records, and talk to family members. One study showed that after just two hours of training and five eight-hour supervised shifts, these technicians hit 92.3% accuracy in collecting medication histories. That’s better than most doctors do on their own.
Then the pharmacist takes over. They compare what the patient says they take, what the hospital says they were given, and what’s in the electronic health record. The system flags anything that doesn’t match - non-formulary drugs, duplicate therapies, expired prescriptions. If a better, cheaper, safer option exists, the pharmacist recommends it. In one hospital, 68.4% of non-formulary medications were switched to formulary alternatives at admission. That’s not just cost savings. It’s fewer side effects and easier access for the patient.
These programs run 7 a.m. to 8 p.m. in most hospitals. In trauma centers, they’re on 24/7. The staffing model? One pharmacist for every three to four technicians. That ratio keeps the workflow moving. Technicians gather data. Pharmacists make decisions. No one is doing both at once. Efficiency matters - each full reconciliation takes about 67 minutes. That’s a lot of time. But when you prevent one hospital readmission, you save more than that in costs.
Why pharmacists - not doctors or nurses - lead this
Doctors are busy. Nurses are stretched thin. Pharmacists? They’re the only ones trained to know every drug interaction, every contraindication, every dosing quirk. A Harris et al. review of 123 studies found that 89% of pharmacist-led programs reduced 30-day readmissions. Only 37% of non-pharmacy-led efforts did. The difference isn’t subtle. It’s massive.
Take the OPTIMIST trial. It compared two groups: one got a simple medication review. The other got a full pharmacist intervention - reconciliation, education, follow-up. The result? The pharmacist group had a 38% lower risk of being readmitted. That’s a hazard ratio of 0.62. The number needed to treat? Just 12. Meaning, for every 12 patients you help this way, you prevent one hospital return.
High-risk patients benefit the most. People over 65. Those on five or more medications. People with low health literacy. For them, a simple miscommunication can mean a fall, a kidney injury, or a trip back to the ER. In one study, patients on the Hospital Readmissions Reduction Program saw a 22% bigger drop in readmissions when pharmacists were involved. That’s not luck. It’s precision.
Deprescribing: The quiet revolution in medication safety
One of the most powerful parts of these programs isn’t adding drugs - it’s taking them away. Deprescribing is the intentional stop of medications that no longer help or might hurt. Think of an 82-year-old on a proton pump inhibitor for heartburn they haven’t had in three years. Or an elderly patient still on an anticholinergic that’s making them confused and unsteady. These aren’t rare. They’re common.
Studies show that in pharmacist-led programs, about half of all recommendations involve stopping a drug. The Beirut study found 52% of substitutions were for discontinuation. That’s huge. And the results? Stopping PPIs cut C. difficile infections by 29%. Cutting anticholinergics reduced falls by 41%. These aren’t minor wins. They’re life-changing.
But here’s the catch: doctors don’t always agree. Physician acceptance of pharmacist recommendations hovers around 30%. That’s the biggest roadblock. Successful programs solve this by embedding the pharmacist directly into the care team. They don’t send emails. They walk into the room. They talk to the doctor. They use the EHR to auto-flag risks. They make it easy to say yes.
The hidden costs - and how to pay for them
These programs don’t run on goodwill. They need people, time, and tech. Each reconciliation takes 67 minutes. Documentation adds another 12.7 minutes. That’s over an hour per patient. Multiply that by 50 patients a day? That’s 60+ hours of pharmacist time. And it’s expensive.
That’s why reimbursement is the biggest hurdle. Only 32 states fully reimburse pharmacist-led substitution services through Medicaid. Medicare Part D covers it for 28.7 million beneficiaries, but the paperwork is a nightmare. Most hospitals absorb the cost because they save more in avoided readmissions. The CMS Hospital Readmissions Reduction Program penalizes hospitals with high readmission rates. In places that run these programs, penalties dropped by 11.3%. That’s real money.
And the market is growing. The U.S. medication reconciliation market hit $1.87 billion in 2022. It’s projected to hit $3.24 billion by 2027. Why? Because value-based care is here. Accountable Care Organizations (ACOs) are now including pharmacist-led substitution metrics in their contracts. That’s a signal: this isn’t a nice-to-have. It’s a must-have.
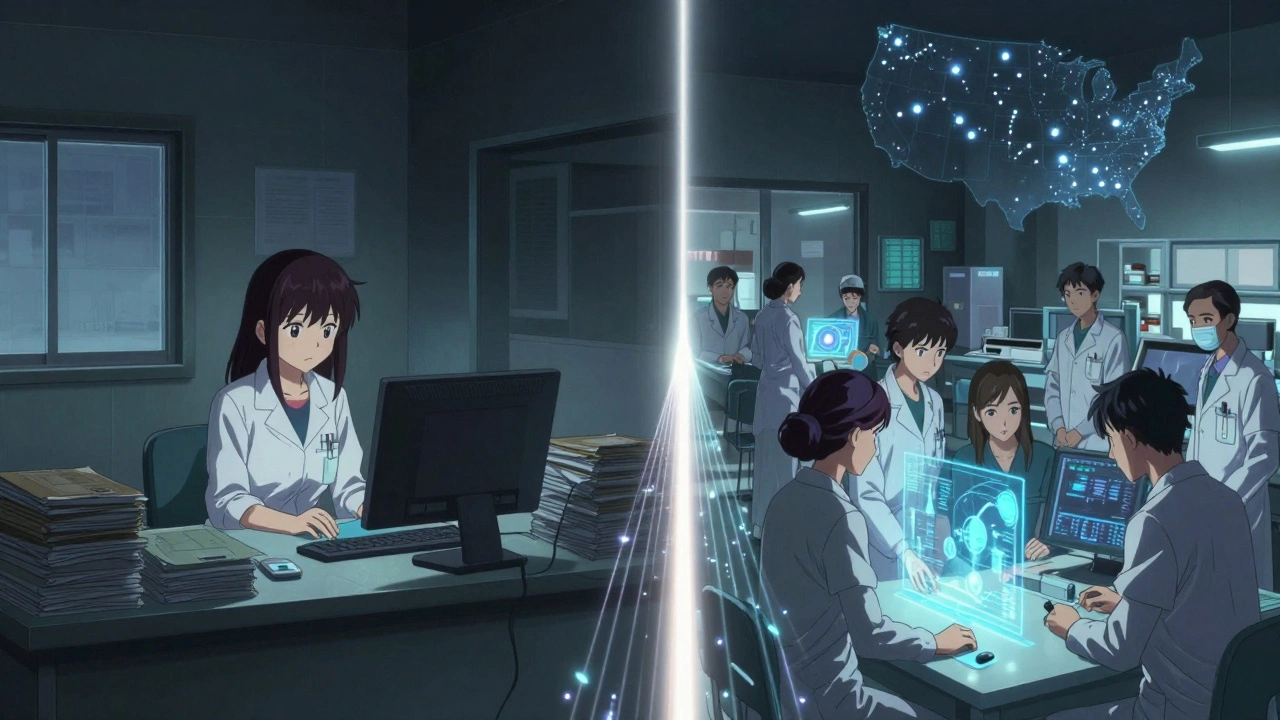
What’s next? AI, policy, and the rural gap
Technology is making these programs faster. AI tools now pull medication histories from pharmacies, insurers, and patient portals - cutting data collection time by 35%. Fourteen academic centers are testing them right now. CMS’s 2024 interoperability proposal could boost reimbursement by 18-22% if pharmacists can document substitutions directly in the EHR.
But not everyone benefits equally. In rural areas, only 22% of critical access hospitals have full programs. Urban academic centers? 89%. Why? Pharmacist shortages. No one to hire. No budget to pay for them. This isn’t just a logistics problem - it’s a justice issue. Patients in small towns get less safe care.
Change is coming. Twenty-seven state pharmacy associations are pushing for expanded substitution authority. The 2022 Consolidated Appropriations Act now requires medication reconciliation for all Medicare Advantage patients - creating a $420 million opportunity. And the Joint Commission now calls pharmacist-led reconciliation a “preferred practice.” That’s not a suggestion. It’s a standard.
What patients and families should know
If you or a loved one is going to the hospital, ask: “Will a pharmacist review all my medications before I leave?” Don’t assume it’s happening. Push for it. Bring a list - even if you think it’s old. Write down every pill, dose, and frequency. Include vitamins, supplements, over-the-counter drugs. Don’t leave it to memory. That’s how errors start.
And if you’re told a medication is being changed or stopped, ask why. Don’t be afraid to question it. Pharmacists are there to protect you. They’re not trying to cut corners. They’re trying to cut risk. If they suggest stopping a drug you’ve been on for years, it’s not because they’re rushing you. It’s because they’ve seen the data. That pill might be doing more harm than good.



Comments (13)
Kyle Flores
I saw this firsthand when my grandma got discharged last year. They caught her still on a muscle relaxant she’d stopped 8 months prior. She was dizzy all the time. Pharmacist fixed it before she even left the hospital. No drama. Just good work.
She’s been stable since. Honestly, why isn’t this standard everywhere?
Ryan Sullivan
Let’s be clear: this is just another example of scope creep disguised as innovation. Pharmacists are not clinicians. They’re dispensers. The notion that they should be leading medication reconciliation is a systemic failure of physician oversight. The data cherry-picks outcomes while ignoring the fact that 30% of their recommendations are rejected because they’re clinically unsound.
Wesley Phillips
Okay but like… why are we still talking about this like it’s revolutionary? 🤡
Pharmacists have been doing this for decades. The fact that hospitals are only now ‘discovering’ it is wild. Also 67 minutes per patient? That’s a whole Netflix episode. Someone’s gotta be doing this while the patient’s still in the bed, right? Or are we just making them wait longer for discharge?
Olivia Hand
The deprescribing stats blew me away. 52% of substitutions were for stopping meds? That’s not just efficiency-that’s ethical. I’ve seen elderly patients on 12+ pills, half of which were for symptoms that disappeared years ago. It’s not care. It’s inertia. And the fact that doctors resist this? That’s the real crisis.
Desmond Khoo
This is literally the most important thing happening in healthcare right now 🙌
My uncle got sent home with 7 new meds after a fall. No one checked if he was still on his old ones. He ended up in the ER again. If this program had been there… he’d still be at home. Thank you to every pharmacist doing this work. You’re the real MVPs 💪💊
Louis Llaine
So let me get this straight. We’re spending $1.87 billion to fix what doctors should’ve done in the first place? And we’re calling it innovation? Brilliant. Let’s just outsource responsibility to people who aren’t legally allowed to diagnose anything. Classic.
Jane Quitain
I work in a rural clinic and we dont even have a pharmacist on staff. We get one for 2 hours a week. My heart breaks for the folks who dont get this. Please dont let this stay a luxury for big hospitals. Everyone deserves to not get poisoned by their own meds 💔
Kyle Oksten
There’s an unspoken assumption here: that patients are passive recipients of care. But what if the real problem is that we’ve normalized medical overreach? Deprescribing isn’t just about safety-it’s about autonomy. We’ve built a system that equates ‘more drugs’ with ‘better care.’ That’s a cultural flaw, not a logistical one.
Sam Mathew Cheriyan
You know who really runs this? Big Pharma. They want you on meds forever. The ‘pharmacist-led’ thing? Total distraction. The real goal is to make you dependent on expensive brand-name drugs. They don’t care if you stop a PPI-they care if you keep buying the new one. This is a smoke screen.
Ernie Blevins
So what? You saved 12 people. Big deal. What about the other 1000 who got discharged with no review? This is just feel-good noise. You’re not fixing the system. You’re patching holes while the whole boat is sinking.
Nancy Carlsen
I’m so proud of the pharmacists in my town who do this. They even call patients at home after discharge to check if they’re confused. One guy told me his wife cried because no one had ever cared enough to ask if she understood her meds. This isn’t just clinical. It’s human. 🤍
Ted Rosenwasser
The OPTIMIST trial’s HR of 0.62? Cute. But did they control for socioeconomic status? Did they account for baseline polypharmacy rates? The statistical significance is thin. Also, 68.4% switching to formulary drugs? That’s not clinical decision-making-that’s cost arbitrage disguised as patient care.
Helen Maples
This isn’t optional. It’s essential. Every hospital system should be mandated to implement this. The data is clear. The cost of inaction is measured in preventable deaths, ER visits, and families broken by avoidable harm. If you’re not doing this, you’re not just behind-you’re negligent.