
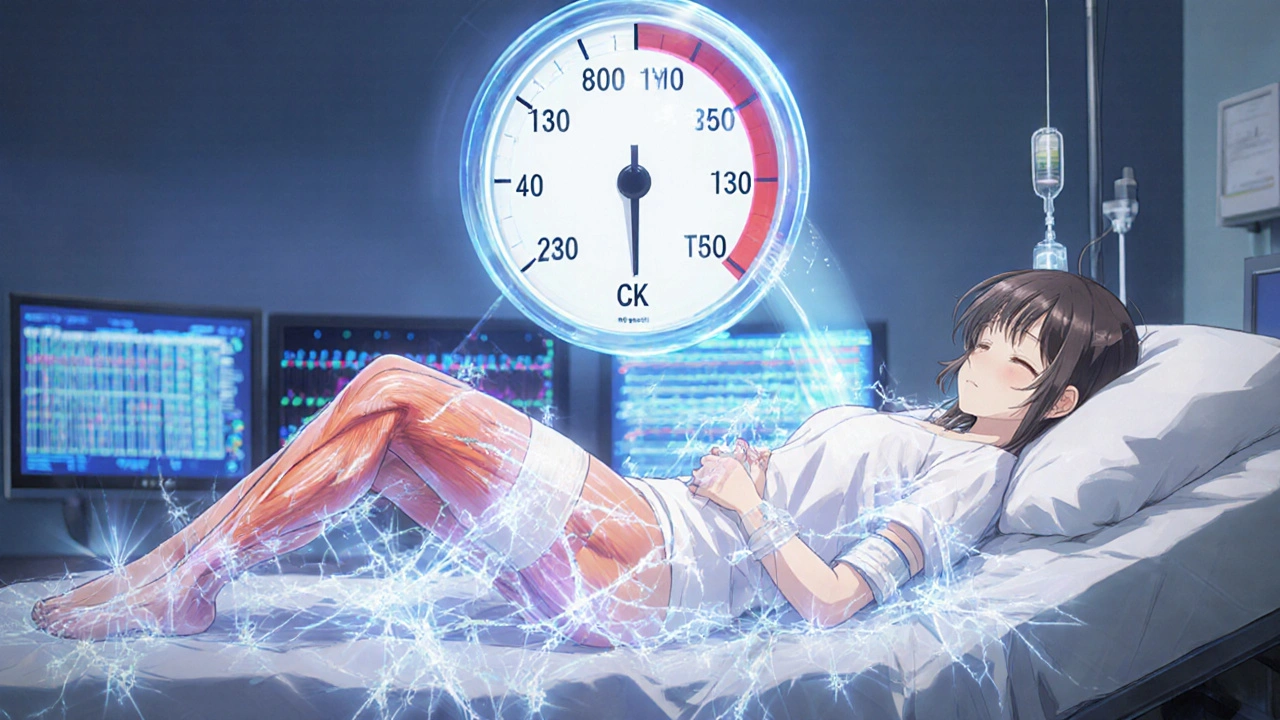
Statins Rhabdomyolysis Risk Calculator
About This Tool
This calculator helps you assess your personal risk of developing rhabdomyolysis while taking statin medications based on factors discussed in the article. Note: This is for educational purposes only and does not replace professional medical advice.
Based on your responses, your risk of rhabdomyolysis is:
Most people taking statins never experience serious muscle problems. But for a tiny fraction, a rare and dangerous condition called rhabdomyolysis can strike - and it can happen fast. If you’re on a statin and suddenly feel your muscles turning to stone, or your urine turns dark like cola, this isn’t just soreness. It’s a medical emergency.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis means your skeletal muscles are breaking down at an alarming rate. When muscle cells die, they spill their contents - including a protein called myoglobin - into your bloodstream. Your kidneys try to filter it out, but myoglobin clogs the tiny tubes inside them. That’s how kidney failure starts. In severe cases, it can lead to dialysis, heart rhythm problems, or even death.Statins cause this in about 1.5 to 5 out of every 100,000 people who take them each year. That’s less likely than being struck by lightning. But when it happens, it’s serious. Most cases show up within the first three months of starting the drug, often after physical activity that pushes the muscles harder than usual.
Why Do Statins Cause Muscle Breakdown?
Statins work by blocking a key enzyme in your liver to lower cholesterol. But that same enzyme is also involved in making other important compounds - ones your muscles need to function properly. When statins interfere, several things go wrong at once.First, they reduce levels of coenzyme Q10 (CoQ10), which your muscles use to make energy. Without enough CoQ10, muscle cells struggle to keep up, especially during exercise. Second, statins trigger a cellular cleanup system called the ubiquitin-proteasome pathway. This system normally removes damaged proteins, but when overactivated, it starts chewing up healthy muscle tissue. Studies show genes like atrogin-1 spike in patients on high-dose statins, turning muscle breakdown into a runaway process.
There’s also evidence that statins - especially the more lipophilic ones like simvastatin and lovastatin - can weaken the outer membrane of muscle cells. Think of it like poking tiny holes in a balloon. When you do eccentric movements - walking downhill, lowering weights, even climbing stairs - the stress on those weakened membranes can cause them to rupture.
Not All Statins Are Created Equal
Your risk depends heavily on which statin you’re taking and how much. Simvastatin at 80 mg carries the highest risk. In fact, the FDA banned new prescriptions of that dose in 2011 after data showed it increased muscle damage risk by more than 10 times compared to 20 mg. Even at lower doses, simvastatin is riskier than others.Pravastatin and fluvastatin are much safer on muscles. Rosuvastatin and atorvastatin fall in the middle. Why? It comes down to how the body processes them. Statins like simvastatin, lovastatin, and atorvastatin are broken down by a liver enzyme called CYP3A4. If you take anything that blocks this enzyme - like clarithromycin (an antibiotic), grapefruit juice, or even some antifungals - your statin levels can spike. One case report showed clarithromycin increased simvastatin levels by 10 times. That’s a recipe for disaster.
Pravastatin and rosuvastatin avoid this trap. They’re cleared through different pathways, so drug interactions are far less likely. If you’re on multiple medications, this is a critical point to discuss with your doctor.
Genetics Play a Bigger Role Than You Think
Some people are genetically wired to be more sensitive to statins. A gene called SLCO1B1 controls how well your liver pulls statins out of your blood. If you have a specific variant - c.521T>C - your liver can’t clear the drug efficiently. That means more statin stays in your bloodstream, hitting your muscles harder.People with two copies of this variant (homozygous) have a 4.5 times higher risk of muscle damage. That’s not rare - about 1 in 10 people carry one copy, and 1 in 100 carry two. Testing for this variant is available through companies like OneOme RightMed, costing around $249. While insurance rarely covers it unless you’ve already had muscle issues, it’s worth considering if you’ve had unexplained muscle pain on statins before.
Who’s Most at Risk?
Age, gender, and health status matter. Most cases occur in people over 65. Women are more likely than men to develop rhabdomyolysis - 62% of reported cases are female. That’s partly because older women often take more medications, increasing interaction risks. People with kidney disease, hypothyroidism, or diabetes are also at higher risk.Physical activity is a major trigger. Patients on forums like Reddit and PatientsLikeMe report the same pattern: crushing leg pain after hiking, inability to climb stairs, or sudden weakness after a workout. Physical therapists have documented cases where even moderate exercise led to muscle breakdown in susceptible individuals. The key isn’t to stop moving - it’s to avoid sudden, intense, or eccentric movements (like downhill running or heavy weight-lowering) when you first start a statin or increase the dose.
What Symptoms Should You Watch For?
Most people on statins get mild muscle aches - that’s common. But rhabdomyolysis has red flags:- Severe muscle pain, especially in the thighs, shoulders, or lower back
- Weakness so bad you can’t stand up or lift your arms
- Dark, tea-colored, or cola-colored urine
- Fever, nausea, vomiting, or confusion
If you have any of these, stop the statin and get medical help immediately. Don’t wait. A simple blood test for creatine kinase (CK) can confirm muscle damage. Levels over 10 times the upper limit mean you need urgent care. If CK hits 10,000 IU/L or higher - and your urine is dark - you’re at high risk for kidney failure. IV fluids and kidney monitoring are critical.
What Happens After Diagnosis?
Once rhabdomyolysis is confirmed, the statin must be stopped. No exceptions. Your doctor will likely check kidney function, electrolytes, and heart rhythm. Hydration is the first line of defense - you’ll need fluids to flush out myoglobin. In severe cases, you might need dialysis.After recovery, restarting a statin is possible - but not with the same drug. Switching to a lower-risk statin like pravastatin or rosuvastatin at a low dose often works. Some patients can even return to their original statin after a long break, but only under strict supervision. Studies show that 78% of people who think they’re statin-intolerant can actually tolerate a different statin or lower dose with proper management.
Alternatives If Statins Are Too Risky
If you truly can’t take any statin, other options exist. PCSK9 inhibitors like alirocumab and evolocumab are injectable drugs that lower LDL cholesterol dramatically - sometimes by 60%. But they cost about $5,850 a year, and insurance often denies them unless you’ve had a heart attack or have familial hypercholesterolemia.Non-statin options like ezetimibe or bempedoic acid are cheaper and carry much lower muscle risk. Bempedoic acid works in the liver, not the muscles, so it’s often well-tolerated. These aren’t as powerful as high-dose statins, but they’re safer for those who can’t tolerate them.
The Bigger Picture: Risk vs. Reward
Let’s be clear: statins save lives. In the U.S., they prevent about 500,000 heart attacks and strokes every year. For someone with a history of heart disease, diabetes, or very high cholesterol, the benefit of taking a statin far outweighs the tiny risk of rhabdomyolysis.The real problem isn’t the drug - it’s the fear. Muscle pain is common, but true rhabdomyolysis is not. Too many people quit statins because of mild aches, then end up having a heart attack they could have prevented. If you have muscle symptoms, don’t assume it’s the statin. See your doctor. Get tested. Rule out other causes like thyroid issues or vitamin D deficiency. Often, the fix is as simple as switching statins or lowering the dose.
What to Do Now
If you’re on a statin:- Know your dose and which one you’re taking. Simvastatin 80 mg is off-limits for new patients - if you’re still on it, ask your doctor why.
- Review all your medications with your pharmacist. Avoid grapefruit juice if you’re on simvastatin, lovastatin, or atorvastatin.
- Start new exercise routines slowly. Avoid downhill running, heavy lifting, or sudden increases in activity.
- Pay attention to urine color. Dark urine is a red flag - don’t ignore it.
- If you have unexplained muscle pain, get your CK checked. Don’t wait for it to get worse.
And if you’ve been told you’re statin-intolerant? Don’t give up. Talk to a cardiologist who specializes in lipid management. There’s almost always a way forward.
Can statins cause muscle damage even at low doses?
Yes, but it’s rare. While higher doses and certain statins like simvastatin carry more risk, even low-dose statins can cause muscle issues in genetically sensitive individuals. The key is not the dose alone - it’s how your body processes the drug, what other medications you’re taking, and whether you’re doing strenuous exercise. If you feel unusual muscle pain at any dose, get it checked.
Is rhabdomyolysis reversible?
Yes, if caught early. Stopping the statin and getting hydrated usually allows muscles to recover fully. Kidney damage can also reverse if treated quickly with IV fluids. But if kidney failure sets in or if the condition goes untreated for days, permanent damage or death can occur. Speed matters.
Should I take CoQ10 supplements to prevent statin muscle pain?
Some people report feeling better taking CoQ10, but studies haven’t proven it prevents rhabdomyolysis. A 2007 trial showed no significant difference in muscle pain between those taking CoQ10 and those taking a placebo. It’s not harmful to try, but don’t rely on it as a solution. If you’re having symptoms, see your doctor - don’t self-treat.
Can I restart a statin after having rhabdomyolysis?
It’s possible, but not with the same drug. Most doctors recommend switching to a low-risk statin like pravastatin or rosuvastatin at the lowest possible dose. Some patients tolerate this well. Never restart without medical supervision. Blood tests for CK should be done before and after restarting.
How do I know if my muscle pain is from statins or something else?
A simple blood test for creatine kinase (CK) can tell you if muscle damage is happening. If CK is normal, your pain is likely from another cause - maybe overuse, arthritis, or nerve issues. If CK is elevated, your doctor will look at your statin type, dose, other meds, and genetic risk factors. Don’t guess - get tested.





Comments (8)
Bonnie Sanders Bartlett
If you're on a statin and notice your urine looks like cola, don't wait. Go to the ER. I saw a neighbor go through this last year-she was fine after fluids and switching statins, but she almost lost her kidneys because she thought it was just soreness from yoga. It's not worth the gamble.
Statins save lives, but listening to your body saves yours.
Melissa Delong
Let me tell you something the pharmaceutical industry doesn't want you to know: statins were never meant to be taken long-term. They're a Band-Aid on a bullet wound. The real cause of heart disease? Sugar, processed foods, and corporate greed pushing pills instead of real nutrition. CoQ10? A distraction. The truth is, your liver isn't broken-it's being poisoned by a system that profits from your fear.
They banned simvastatin 80mg? Of course they did. After enough people started dying. They'll never admit they knew all along.
Marshall Washick
I started on atorvastatin last year after my LDL hit 190. Mild muscle ache at first-I ignored it. Then, after a long hike, I couldn’t lift my arms. Dark urine. I went to urgent care. CK was 12,000.
Turns out I’m SLCO1B1 positive. Switched to pravastatin 10mg. No issues since. I didn’t quit statins-I just found the right one. If you’re scared, talk to a lipid specialist. Don’t assume it’s over for you.
Abha Nakra
As someone from India, I’ve seen this play out differently here. Many patients are on low-dose statins because of cost, not because they’re safer-but the genetic risk is the same. SLCO1B1 variants are actually more common in South Asian populations than in Caucasians.
And yes, grapefruit juice is a silent killer here too-people drink it daily thinking it’s ‘healthy.’ I’ve seen three cases in my clinic alone where someone was on simvastatin and drank grapefruit juice every morning. One ended up in dialysis.
Knowledge is power. Share this with your family.
Neal Burton
It’s amusing how casually people dismiss rhabdomyolysis as ‘rare.’ Rare doesn’t mean impossible-it means it happened to someone who wasn’t warned. And let’s not pretend the FDA’s actions were altruistic. They acted because lawsuits were piling up, not because they cared about your muscles.
CoQ10 supplements? A $30/month placebo for people too afraid to confront the truth: statins are a gamble with your body’s biochemistry. The fact that you’re even considering supplements means you already know something’s off.
Tamara Kayali Browne
Let’s quantify the risk properly. The annual incidence of rhabdomyolysis from statins is 1.5–5 per 100,000. That’s 0.0015% to 0.005%. The risk of dying from a heart attack if you have coronary artery disease and don’t take a statin? Over 10% per year.
Comparing these numbers isn’t fearmongering-it’s epidemiology. The media amplifies rare outcomes because they’re sensational. The real tragedy isn’t rhabdomyolysis-it’s people abandoning life-saving therapy because they read a Reddit thread.
Nishigandha Kanurkar
Wait-so you’re telling me the same drug that’s supposed to protect your heart is secretly eating your muscles?! And they don’t test you before prescribing?! And grapefruit juice is a TRAP?! And they don’t even tell you about the gene test?!
THIS IS A COVER-UP! Big Pharma doesn’t want you to know you can be genetically doomed by a pill you took for ‘cholesterol’! My cousin took simvastatin and ended up in ICU-no warning, no testing, no nothing! They’re poisoning us with pills and calling it ‘medicine’!
GET TESTED! Demand SLCO1B1 testing! Demand alternatives! Don’t let them turn your body into a chemical experiment!
Lori Johnson
My mom was told she was statin-intolerant after mild soreness. She quit cold turkey. Six months later, she had a stroke. Turns out her LDL was 220 and she had a family history. She switched to ezetimibe and now she’s fine.
Don’t give up on statins-just find the right one. And yes, check your meds with your pharmacist. I didn’t know my blood pressure pill interacted with her statin until I asked. That one conversation saved her life.
You’re not alone. Just don’t panic. Talk. Test. Switch. You’ve got this.