
Corticosteroid Taper Calculator
According to the article, abrupt cessation of steroids beyond 2-4 weeks can cause adrenal insufficiency in up to 78% of patients.
The article recommends slow tapering below 15 mg daily to avoid withdrawal symptoms.
Stopping corticosteroids like prednisone isn’t as simple as taking your last pill and calling it quits. If you’ve been on these medications for more than a few weeks, your body has stopped making its own cortisol. Suddenly cutting them out can trigger a cascade of symptoms-fatigue so deep it feels like you’re dragging through wet concrete, muscle aches, nausea, and even panic attacks. This isn’t just "feeling off." It’s your adrenal glands screaming for time to wake up. The solution? A carefully planned corticosteroid taper.
Why Tapering Isn’t Optional
When you take corticosteroids for longer than 2-4 weeks at doses above 7.5 mg of prednisone daily, your brain tells your adrenal glands to shut down cortisol production. It’s like putting your body on autopilot. You’re giving it an external supply, so it figures, "No need to work." But when you stop abruptly, your adrenals don’t snap back to life. They’re asleep. And your body doesn’t know how to cope.Studies show that 78% of people who quit cold turkey experience withdrawal symptoms. That’s nearly four out of five. Symptoms include:
- Severe fatigue that doesn’t improve with rest
- Joint and muscle pain, often mistaken for arthritis flare-ups
- Nausea, vomiting, or loss of appetite
- Mood swings, anxiety, or depression
- Sleep disturbances and brain fog
These aren’t "side effects." They’re signs your body is starving for cortisol. Without tapering, you risk adrenal insufficiency-a medical emergency that can lead to low blood pressure, confusion, and even collapse.
How Fast Should You Taper?
There’s no one-size-fits-all schedule. Your taper depends on how long you’ve been on steroids, your dose, and what condition you’re treating-like rheumatoid arthritis, lupus, or Crohn’s disease.For those on high doses (over 20 mg of prednisone daily), doctors often start with a faster drop: reduce by 2.5 to 5 mg every 3 to 7 days. Once you hit 15 mg, things slow down. From there, drop by 1 mg every 1 to 2 weeks. Why? Because below 15 mg, your body starts reacting. Around 63% of patients report symptoms when doses fall below this level.
When you get to 5-7.5 mg-the level your body naturally produces-you’re in the final stretch. This is where patience matters most. Going too fast here can trigger a full-blown withdrawal crisis. Some people need weeks just to go from 5 mg to 0 mg.
For those on long-term therapy (over a year), tapering can take 6 to 12 months. It’s not a race. It’s a recovery process.
Differentiating Withdrawal, Flare, and Insufficiency
This is where things get tricky. Many patients and even some doctors confuse three very different things:- Withdrawal syndrome: Generalized fatigue, achiness, nausea, mood changes-no inflammation markers.
- Disease flare: Your original condition comes back with force-swollen joints in RA, diarrhea in Crohn’s, rash in lupus.
- Adrenal insufficiency: Dangerously low cortisol. Signs include dizziness when standing, low blood pressure, low sodium, low blood sugar.
Doctors can test for adrenal insufficiency with a cosyntropin (ACTH) stimulation test. A normal response means your cortisol level jumps above 400-500 nmol/L within an hour. If it doesn’t, you still need steroid support.
Here’s the scary part: 34% of people who think they’re having a disease flare are actually just going through withdrawal. And if you’re given more steroids because of that misdiagnosis, you’re stuck in a loop.
What Helps During Tapering?
Tapering isn’t just about reducing pills. It’s about supporting your body as it relearns how to function on its own.Exercise: A 2022 study in Rheumatology found that 20 minutes of daily walking or warm-water pool therapy cut muscle and joint pain by 42%. Movement helps your body adjust.
Physical therapy: Patients in one trial saw their pain scores drop from 7.2 to 3.1 on a 10-point scale in just four weeks with guided rehab.
Cognitive behavioral therapy (CBT): Anxiety and depression during tapering are real. A 2023 trial by the American Addiction Centers showed CBT reduced psychological symptoms by 68% compared to no intervention.
Diet and sleep: The Mayo Clinic tracked over 1,200 patients. Those who ate a Mediterranean-style diet (lots of veggies, fish, olive oil), limited caffeine to under 200 mg a day (about two cups of coffee), and slept 7-9 hours nightly saw a 55% drop in symptom severity.
Even with all this, 22% of people still need to temporarily raise their dose. That’s not failure. It’s fine-tuning.
What Patients Are Really Saying
Reddit’s r/Prednisone community has over 12,500 members. A majority-68%-say they still got withdrawal symptoms even with a "prescribed" taper. Forty-one percent describe crushing fatigue that lasted 3 to 8 weeks. On Drugs.com, the average symptom duration was 22.7 days. For 18%, it dragged on past 60 days.The biggest complaints? Doctors didn’t explain the process clearly (76%), tapering schedules changed without reason (63%), and no one talked about the mental toll (52%).
Those who did well? They had a written plan, stuck to it, and got support from physical therapists and counselors. One 45-year-old woman with rheumatoid arthritis tapered from 40 mg to 0 mg over 26 weeks using a European protocol-and had zero symptoms.
What You Need to Do
If you’re on corticosteroids and your doctor says it’s time to taper, here’s your action list:- Get a written tapering schedule-don’t rely on memory or vague instructions.
- Ask for a steroid emergency card. It should list your highest dose and what to do if you get sick, injured, or have surgery.
- Learn to check your orthostatic blood pressure: lie down for 5 minutes, stand up, measure your systolic pressure. If it drops more than 20 mmHg, call your doctor.
- Track your symptoms daily. Note fatigue, pain, mood, sleep. This helps your doctor spot patterns.
- Ask for a referral to physical therapy or a counselor if you’re struggling.
- Never skip a dose or speed up the taper without talking to your provider.
Most importantly: don’t feel guilty if you need to slow down. Tapering isn’t a test of willpower. It’s a biological reset. Rushing it risks hospitalization. The Endocrine Society says 89% of corticosteroid-related ER visits come from improper tapering.
What’s New in 2025?
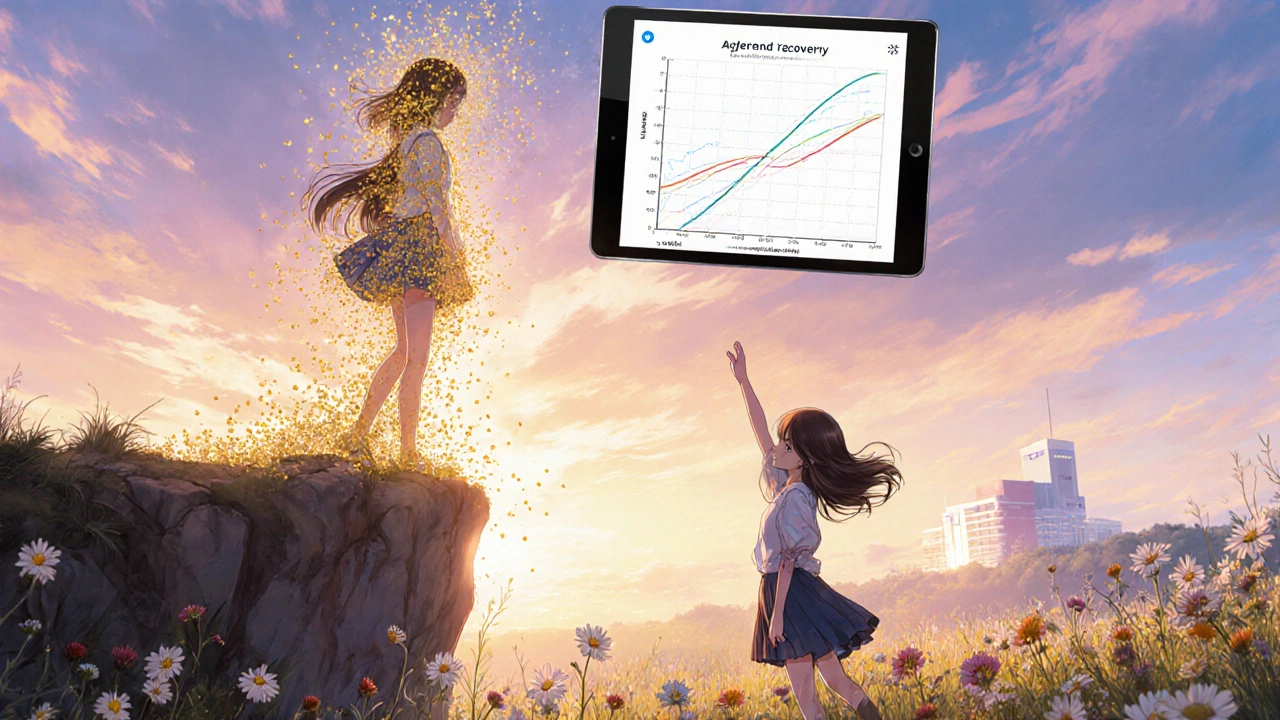
The field is changing. In March 2024, Mayo Clinic launched a digital tapering assistant that tracks symptoms and adjusts schedules automatically. In their pilot study, it cut complications by 37%.Researchers are now using salivary cortisol tests-measuring your natural morning spike-to predict how fast your HPA axis recovers. Early results show 82% accuracy in forecasting recovery time.
AI-driven tapering tools are in clinical trials at Johns Hopkins. These systems pull data from your EHR-meds, lab results, activity levels-to create a personalized plan. By 2027, experts predict standardized protocols could prevent over 200,000 emergency visits a year in the U.S. alone.
But access is still unequal. Rural patients have 2.3 times more complications than urban ones. If you’re in a remote area, ask about telehealth endocrinology visits. Your recovery shouldn’t depend on your zip code.
Final Thought
Corticosteroids save lives. But they also leave a mark. Tapering isn’t the end of treatment-it’s the beginning of healing. It’s not about getting off the drug. It’s about getting your body back.Be patient. Be loud. Be persistent. If your doctor won’t give you a clear plan, ask for a referral to an endocrinologist. You deserve to come off these meds without suffering.
How long does corticosteroid withdrawal last?
Withdrawal symptoms usually start within a few days of reducing your dose and can last from a few weeks to several months. Most people feel better within 4 to 8 weeks, but those who were on long-term therapy (over a year) may experience fatigue or joint pain for 3 to 6 months. The key is pacing the taper slowly-rushing it only makes symptoms worse and longer-lasting.
Can I taper off prednisone on my own?
No. Tapering corticosteroids without medical supervision is dangerous. Your body may not be able to restart cortisol production, leading to adrenal insufficiency-a life-threatening condition. Even if you feel fine, your adrenal glands might still be shut down. Always follow a doctor-approved plan with regular check-ins.
What’s the difference between withdrawal and a disease flare?
Withdrawal symptoms are general: fatigue, muscle aches, nausea, mood changes. A disease flare is specific to your condition. For example, if you have rheumatoid arthritis, a flare means swollen, hot joints. If you have Crohn’s, it’s diarrhea and abdominal pain. Blood tests and symptom patterns help doctors tell the difference. Never assume it’s a flare without checking.
Do I need blood tests during tapering?
Not always, but they’re important if you’re having symptoms at low doses (below 5 mg). A cosyntropin stimulation test measures your adrenal response and confirms whether your HPA axis is recovering. If your cortisol doesn’t rise enough, you may need to slow the taper or temporarily increase your dose.
What should I do if I miss a dose during tapering?
Don’t double up. If you miss a dose, take it as soon as you remember-if it’s within a few hours. If it’s later in the day, skip it and continue with your next scheduled dose. Abruptly skipping doses can trigger withdrawal. Call your doctor if you miss more than one dose or feel unwell. Keep your emergency card handy in case you need urgent care.
Can I use natural supplements to help with withdrawal?
There’s no proven supplement that replaces cortisol or speeds up HPA axis recovery. Some people try licorice root or ashwagandha, but these aren’t backed by strong evidence and can interfere with medications. Focus on proven supports: sleep, nutrition, exercise, and therapy. Never replace medical advice with supplements-especially when your adrenal system is vulnerable.
Will my adrenal glands ever recover fully?
Yes, in most cases. Recovery time depends on how long you were on steroids. People on short-term therapy (under 3 weeks) usually bounce back in 1-2 weeks. For those on long-term treatment (over a year), full recovery can take 6 to 12 months. Even then, your body may remain more sensitive to stress for a while. That’s why carrying an emergency card is still recommended, even after you’ve stopped.
What’s the lowest dose I can safely stop at?
The goal is to reach zero, but only if your body can handle it. Most people stop at 0 mg after a slow taper. However, some patients with chronic conditions may need to stay on a very low maintenance dose (like 2.5 mg prednisone every other day) to prevent flares. Your doctor will help you find the balance between safety and disease control. Never stop abruptly, even at 0.5 mg.
Are there alternatives to tapering?
There are no direct alternatives to tapering if you’ve been on corticosteroids long-term. But you can reduce your dependence by switching to non-steroidal treatments-like biologics for autoimmune diseases, or disease-modifying drugs for arthritis. Work with your specialist to find long-term alternatives before you start tapering. This makes the process smoother and safer.
What should I do if I feel worse after stopping?
Don’t panic, but don’t ignore it. Contact your doctor immediately. You may need to temporarily restart a low dose and taper slower, or you may have adrenal insufficiency. Symptoms like dizziness, fainting, vomiting, or confusion require urgent care. Keep your emergency card with you at all times until your doctor confirms your adrenals are fully recovered.





Comments (13)
Robert Bowser
Just finished my 14-month taper from 40mg to 0. It was brutal, but the key was writing down every symptom and sharing it with my endo. No one told me how much mental fog would hit-like my brain was wrapped in saran wrap. I thought I was going crazy, but it was just my HPA axis rebooting. Walked 20 minutes daily. No caffeine after noon. Sleep was non-negotiable. I’m 8 months off and finally feel like myself again.
Krishna Kranthi
Bro in India here, my cousin went through this last year-doc gave him a 6-week taper from 20mg and he ended up in ER with low BP. Turns out his doc didn’t even know about the cosyntropin test. We had to drag him to a private endo who actually listened. Now he’s on a 10-month plan. Lesson? Don’t trust just any doctor. Find someone who gets it. And yes, the fatigue hits harder than a Mumbai monsoon.
Lilly Dillon
I tapered from 10mg over 11 months. The worst part wasn’t the pain-it was the guilt. Like I was failing because I still felt tired. Everyone says 'just push through' but your body isn’t a car you can just rev up. I cried more than I ever have. Took therapy. It helped more than I expected.
Shiv Sivaguru
Why are we even doing this? Corticosteroids are just a bandaid. The real issue is pharma pushing pills instead of fixing root causes. Why not just fix the immune system instead of suppressing it? You're just trading one problem for another. And now you're stuck in this 18-month detox hell? This system is broken.
Gavin McMurdo
Let me get this straight-you’re telling me we’re supposed to believe that a 22.7-day average symptom duration is somehow "normal"? That’s not recovery, that’s a medical failure. And now we’re supposed to trust an "AI-driven tapering assistant"? Next they’ll be implanting cortisol chips. This whole thing smells like Big Pharma’s way of keeping patients dependent on the system. The Endocrine Society? Please. They’re funded by the same companies that make prednisone.
Jesse Weinberger
So you're telling me if I just walk and eat kale I can fix my adrenal glands? Lol. I've been on prednisone for 3 years. My body doesn't make cortisol anymore. No amount of yoga or green smoothies is gonna change that. And don't get me started on CBT-like my anxiety is just "in my head"? Nah. My adrenals are dead. And your "68% reduction"? That's just stats. I'm the 32% who still can't get out of bed.
Emilie Bronsard
This is the most helpful post I’ve read in years. Thank you for explaining the difference between flare and withdrawal. I thought I was failing my RA treatment. Turns out I was just healing.
John Bob
AI-driven tapering tools? That’s a joke. They’re using your EHR data to predict your cortisol recovery? Who gave them access? This is surveillance medicine. Your doctor doesn’t care about your recovery-they care about your insurance codes. And that "emergency card"? It’s a trap. They want you to panic and come back for more steroids. Don’t fall for it.
Alex Grizzell
YOU GOT THIS. 🙌 I tapered from 30mg over 10 months. Had days I wanted to quit. But I kept a journal. I celebrated every 1mg drop like it was a birthday. I found a Reddit group that didn’t judge. You’re not weak for needing time. You’re brave for trying. Keep going. You’re not alone.
George Johnson
They say 89% of ER visits come from improper tapering. Funny how they never mention that 89% of those patients had doctors who gave them a one-page printout and said "good luck."
Rodrigo Ferguson
One must question the epistemological foundations of this medical paradigm. The assumption that cortisol replacement via exogenous administration is a therapeutic endpoint rather than a symptomatic palliation reveals a profound ontological failure within contemporary endocrinology. The HPA axis is not a circuit to be calibrated-it is a living, dynamic system whose integrity is compromised by pharmacological hegemony. One must therefore inquire: Who benefits from the institutionalization of the taper? And at what cost to human autonomy?
Mickey Murray
Look, I get it. You want to feel better. But you’re not special. Everyone who’s ever taken steroids goes through this. The fact that you’re surprised means you didn’t read the damn label. And now you want a therapist and a physical therapist and an AI assistant? Get a grip. This isn’t a spa retreat. It’s medicine. Suck it up. And stop treating your body like a fragile doll.
Marcia Martins
I’m 3 months off and still get dizzy when I stand up. My doctor said "it’ll pass." But I didn’t feel heard. Then I found a nurse practitioner who actually listened. She adjusted my taper by 0.5mg and gave me electrolytes. That tiny change made all the difference. If your doctor won’t listen-find someone who will. You deserve that.