
Drug shortages aren’t just inconvenient-they’re dangerous. In 2024, the U.S. Food and Drug Administration recorded over 300 active drug shortages, including life-saving medications like insulin, chemotherapy agents, and antibiotics. Patients delay treatments. Clinicians scramble for alternatives. Hospitals ration doses. And behind every shortage is a broken supply chain, fragile manufacturing, and a system still playing catch-up.
Why drug shortages keep happening
It’s not one problem-it’s a chain reaction. Most shortages start with a single manufacturer unable to produce a drug. Maybe their facility failed an FDA inspection. Maybe raw materials got stuck in port. Maybe a plant had a power outage. But when one company makes 70% of a generic injectable, like phenylephrine or sodium bicarbonate, one hiccup means nationwide scarcity.
Generic drugs are the biggest culprits. They’re cheap, so profit margins are thin. Manufacturers don’t invest in backup equipment or multiple production lines. When demand spikes-like during flu season or a pandemic-there’s no buffer. And because these drugs aren’t patented, no one has an incentive to build extra capacity.
Global supply chains make it worse. Over 80% of active pharmaceutical ingredients (APIs) for U.S. drugs come from China and India. Political tensions, trade restrictions, or natural disasters overseas can cut off supply overnight. In 2023, a flood in a key Indian API facility caused a 12-week shortage of metformin, affecting over 10 million diabetic patients.
What hospitals are doing right now
Health systems aren’t waiting for Washington to fix this. They’re acting locally-with real tools, real data, and real teamwork.
First, they’re building smarter inventory systems. Instead of just ordering based on last month’s usage, top hospitals now use predictive analytics. Mayo Clinic’s pharmacy team uses machine learning to forecast demand down to the daily level, factoring in seasonal trends, patient volume, and even weather patterns that affect ER visits. Their stockouts for critical drugs dropped by 41% in 2024.
Second, they’re sharing resources. Regional drug shortage task forces are forming. In the Midwest, 14 hospital systems now pool their inventory through a shared digital platform. If one hospital runs low on epinephrine, another can transfer it within hours. No more calling 10 pharmacies across three states.
Third, they’re diversifying suppliers. Instead of relying on one vendor for a single generic, hospitals now approve two or three manufacturers-even if they cost 15% more. The extra cost is worth it. In 2024, Cleveland Clinic switched from a single-source supplier of norepinephrine to two approved vendors. When the first supplier had a production delay, the second picked up 90% of the demand without disruption.
Alternative drugs and clinical protocols
When a drug disappears, doctors don’t just guess what to use. They follow evidence-based substitution protocols.
For example, when the supply of propofol dropped in early 2024, anesthesia teams at Johns Hopkins turned to ketamine-midazolam combinations. They didn’t wing it-they ran a retrospective study on 800 past cases, confirmed safety profiles, and published a quick-reference guide for all staff. Within two weeks, every OR had the new protocol printed and posted.
Hospitals are also using compounding pharmacies more. These labs can mix small batches of drugs that aren’t available commercially. The FDA has relaxed rules slightly to allow this during shortages. In 2025, over 200 U.S. hospitals now partner with accredited compounding labs for critical injectables like dopamine, vasopressin, and heparin.
And it’s not just about swapping drugs. Some systems are changing how they use them. At Kaiser Permanente, nurses now give lower doses of certain antibiotics over longer periods when supply is tight. Clinical trials showed it’s just as effective-and they’ve cut usage by 28% without hurting outcomes.

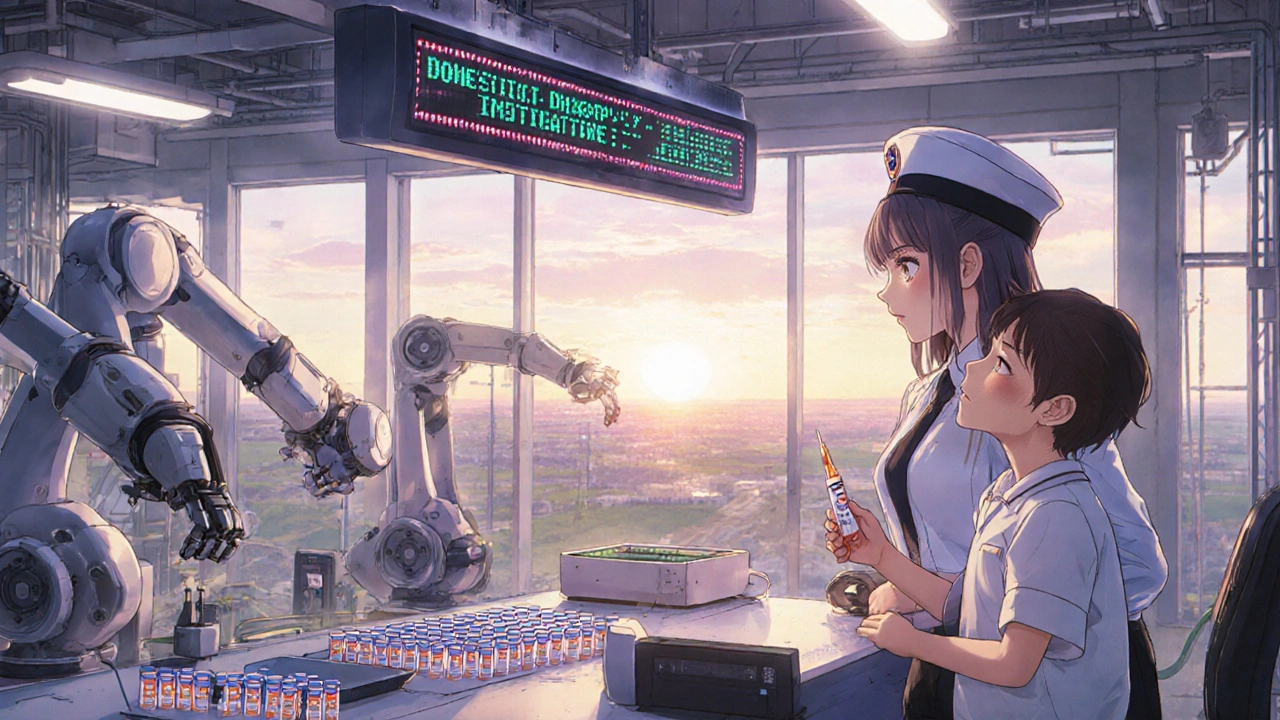
Technology is stepping in
AI isn’t just for chatbots anymore. It’s now helping pharmacists track drug availability in real time.
One health system in Texas uses an AI tool called DrugTrack that scans FDA alerts, manufacturer notices, pharmacy inventories, and even social media reports from nurses on the floor. It flags potential shortages 3-5 weeks before they hit the shelves. That gives pharmacists time to reorder, find alternatives, or adjust schedules.
Robotic dispensing systems are also helping. At Intermountain Healthcare, automated cabinets now prioritize high-risk drugs. If a nurse pulls a vial of insulin, the system checks inventory levels and automatically triggers a reorder if stock falls below a threshold. It doesn’t wait for someone to notice it’s low.
And blockchain is being tested for traceability. A pilot project in California links every batch of a critical drug from manufacturer to bedside. If a recall happens, they know exactly which patients received it-and which ones didn’t. No more guessing.
Long-term fixes: fixing the system, not just the symptom
Short-term fixes help. But real change needs structural shifts.
Some health systems are investing in domestic manufacturing. In 2024, the U.S. government launched the Domestic Drug Supply Initiative, offering grants to build new API facilities. Ten hospitals joined forces to fund a new plant in Ohio that now produces 12 high-demand generics. It’s not cheap-but it’s reliable.
Others are working with insurers to change payment models. Instead of paying per dose, some payers now reimburse based on patient outcomes. That gives hospitals an incentive to use drugs more efficiently, avoid waste, and choose alternatives wisely.
And there’s growing pressure on Congress. The Preserving Access to Life-Saving Medications Act, introduced in early 2025, would require manufacturers to report potential shortages six months in advance-and give the FDA power to fast-track approvals for backup suppliers. Health systems are lobbying hard for it.
What’s still broken
Progress is real-but uneven. Rural hospitals still get left behind. They don’t have the staff to run predictive analytics. They can’t afford AI tools. Their pharmacy teams are one person deep.
And generics are still treated like commodities. Until manufacturers are paid enough to build redundancy into their systems, shortages will keep coming. A single vial of a generic drug might cost $0.50-but the cost of a patient being delayed treatment? That’s measured in lives.
There’s also a cultural problem. Too many clinicians still think, “Someone else will fix it.” But when the drug runs out, it’s the nurse on the floor who has to find a solution. The pharmacist who calls every distributor in the state. The doctor who has to explain to a cancer patient why their chemo is delayed.
The path forward
The best health systems don’t rely on one fix. They stack solutions:
- Use AI to predict shortages before they happen
- Build multi-vendor supply chains for critical drugs
- Train staff on safe alternatives with published protocols
- Partner with other hospitals to share inventory
- Invest in domestic manufacturing where possible
- Push for policy changes that require transparency and accountability
There’s no magic bullet. But when hospitals act together-with data, collaboration, and urgency-they can keep patients safe even when the supply chain cracks.
Drug shortages won’t disappear overnight. But they don’t have to be a crisis every time.
What causes most drug shortages?
Most drug shortages start with a single manufacturer unable to produce a drug due to quality issues, equipment failure, or raw material shortages. Generic drugs are especially vulnerable because they have low profit margins, so manufacturers rarely invest in backup production lines. Over 80% of active ingredients come from overseas, making supply chains fragile to global disruptions.
How do hospitals find alternatives when a drug is out of stock?
Hospitals use evidence-based substitution protocols developed by clinical pharmacists and physicians. These are tested in internal studies and published as quick-reference guides. Many also partner with accredited compounding pharmacies to make small batches of unavailable drugs. AI tools help flag safe alternatives based on patient history and drug interactions.
Can AI really help prevent drug shortages?
Yes. AI tools like DrugTrack scan FDA alerts, manufacturer notifications, and real-time inventory data to predict shortages weeks in advance. Hospitals using these systems have reduced unexpected stockouts by up to 40%. They also automate reordering and flag high-risk drugs before they hit critical levels.
Why aren’t more generic drugs made in the U.S.?
Making generic drugs in the U.S. is expensive, and profit margins are tiny. Most manufacturers rely on low-cost overseas production. But new government grants and hospital-led partnerships are starting to change that. In 2024, a consortium of 10 hospitals funded a new U.S.-based facility that now produces 12 critical generics locally.
What can patients do if their medication is in short supply?
Patients should never switch or stop medications on their own. Instead, they should contact their pharmacy and provider immediately. Pharmacies often know about shortages before patients do and can help find alternatives or arrange transfers from other locations. Some hospitals also offer patient assistance programs to help with access during shortages.




Comments (14)
Ragini Sharma
lol so we paying 50 cents for a vial but some kid in ohio dies cause no insulin?? what a system 😒
Suzan Wanjiru
The compounding pharmacies are a lifesaver but most don't have the license for sterile injectables. FDA needs to fast track more of these labs or we're just patching a leaky boat
Henrik Stacke
I work in a UK NHS trust-we’ve had similar issues with benzylpenicillin. The difference? We negotiate bulk contracts at national level. No hospital fights alone. Maybe the US needs a centralized procurement body for generics.
Kezia Katherine Lewis
The supply chain fragility is a textbook case of market failure. When price elasticity is near zero for life-saving agents, the invisible hand becomes a limp wrist. Regulatory arbitrage has created a structural vulnerability that no amount of AI can fix without upstream intervention.
Linda Rosie
This is exactly why we need to stop treating medicine like a commodity.
JD Mette
I’ve seen nurses cry because they couldn’t get dopamine for a code blue. No one talks about that part.
Vivian C Martinez
The predictive analytics at Mayo are impressive but only work if you have good data and staff who actually use it. In smaller hospitals, someone’s still using Excel sheets from 2018. Tech helps-but only if you invest in the people behind it too.
Ross Ruprecht
All this fancy AI stuff is just corporate theater. The real problem? Pharma CEOs make millions while nurses scramble for vials. Fix the incentives or shut up about algorithms.
Jennifer Shannon
You know what’s wild? We’ve got satellites that can track weather patterns on Mars, but we can’t reliably predict when a hospital in rural Kansas will run out of insulin. It’s not a technical problem-it’s a moral one. We’ve prioritized profit over presence, efficiency over empathy, and shareholder returns over survival. And now we’re surprised when people die because a vial didn’t arrive on time? This isn’t a shortage. It’s a betrayal.
Demi-Louise Brown
The regional inventory sharing model is the most promising development I've seen in years. It's practical, scalable, and human-centered. We need to fund this at the federal level-not as a pilot, but as infrastructure.
Olanrewaju Jeph
In Nigeria we don't have this problem because we don't rely on single-source suppliers. We buy from five different countries and rotate. It's more expensive but we never go without. The lesson? Redundancy isn't optional-it's survival.
Manjistha Roy
The fact that compounding pharmacies are being used as a stopgap instead of a standard practice speaks volumes. We should be incentivizing local compounding as part of every hospital's emergency preparedness plan-not waiting for a crisis to activate it.
Bryson Carroll
AI tools are just glorified spreadsheets with buzzwords. The real issue? No one in Congress has ever held a vial of insulin while watching a diabetic patient go into DKA because the shipment was delayed by a customs glitch in Mumbai. Until the people making the rules feel the consequences, nothing changes
Jennifer Skolney
This is why I started volunteering at my local hospital pharmacy. We’re not waiting for Washington. We’re making lists, calling other clinics, and teaching nurses the alternatives. It’s messy. It’s exhausting. But it works. 🫶