
It’s 2026, and you’re on a routine refill for your generic lisinopril - the cheap, effective blood pressure pill your doctor prescribed. You walk into the pharmacy, hand over your card, and wait. But instead of handing you the bottle, the pharmacist says, "We need prior authorization for this." You blink. Wait, what? It’s a generic. It’s supposed to be the cheap option.
This isn’t a glitch. It’s becoming normal. Even though generics make up 90% of all prescriptions filled in the U.S., more than 1 in 5 now require insurance approval before you can get them. That’s up from just 5% in 2018. And it’s happening to the very drugs meant to save you money.
Why Are Generic Drugs Being Held Up?
Prior authorization was never meant for generics. Back in the 90s, it was created to stop overuse of expensive brand-name drugs and specialty meds. The idea was simple: if a cheaper generic exists, use it. But now, insurers are turning the system upside down. Even when a generic is the first-line treatment, some insurance plans demand paperwork before they’ll pay.
Why? It’s not always about cost control - it’s about formulary management. Pharmacy benefit managers (PBMs), who run drug coverage for insurers, sometimes push for step therapy: you must try one generic before they’ll cover another, even if both are equally effective. Or they’ll restrict access to certain generics within a drug class to steer patients toward ones that give them higher rebates. This isn’t about safety. It’s about profit.
Take metformin, the go-to drug for type 2 diabetes. In 2024, a Kaiser Family Foundation case study found a patient faced a 14-day delay getting their generic metformin because of prior authorization. Their HbA1c - a key diabetes marker - jumped from 6.8% to 8.2% during that wait. That’s not just inconvenient. That’s dangerous.
Who’s Doing This - And Who’s Saying No?
Not all insurers treat generics the same. Aetna requires prior authorization for 25% of its generic medications. UnitedHealthcare, 22%. Humana, 18%. But it’s not random. Certain drug classes are targeted more than others. Oncology generics? 35% require approval. Cardiovascular generics? Only 12%. Why? Because cancer drugs are expensive, and insurers worry about off-label use or higher-cost alternatives being requested.
Meanwhile, some states are pushing back. California’s SB 1024, effective January 2025, bans prior authorization for 47 generics on its Essential Drug List - including common ones like levothyroxine, amoxicillin, and metoprolol. Thirty-four states now restrict prior authorization for certain generic classes. And in December 2023, Congress passed the Improving Seniors’ Timely Access to Care Act, which will require Medicare Advantage plans to process prior authorizations electronically and respond to urgent requests within 72 hours by 2026.
On June 23, 2025, six major insurers - including CVS Health (Aetna), UnitedHealthcare, Cigna, Humana, Elevance Health, and Blue Cross Blue Shield - announced they’d eliminate prior authorization for 12 common generic drug classes by January 2026. That includes ACE inhibitors, statins, and metformin. It’s a win. But it’s only a start.
How It Actually Works - And How to Survive It
If your generic requires prior authorization, here’s what happens next:
- Your doctor’s office gets notified by the pharmacy or insurer that the drug needs approval.
- They submit paperwork - usually electronically through systems like CoverMyMeds - with your diagnosis code (ICD-10), medical history, and sometimes lab results.
- The insurer reviews it. If it’s urgent, they’re supposed to respond in 72 hours. If not, it could take 5-10 business days - or longer.
- If denied, your doctor can appeal with more documentation. About two-thirds of denials get overturned with a proper appeal.
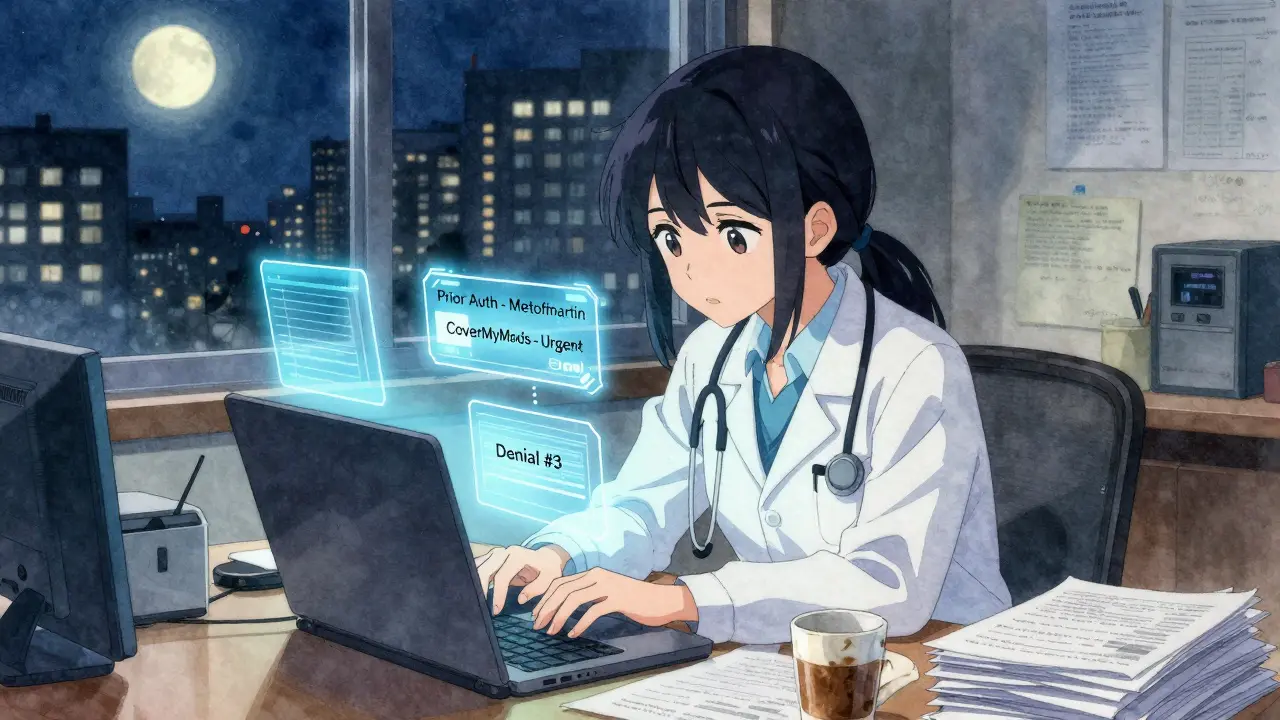
Doctors aren’t sitting idle. A 2024 study in the Journal of the American Pharmacists Association found that electronic submissions cut approval time by 32% compared to fax or phone. But here’s the catch: physicians are spending an average of 43 prior authorizations per week. Nearly 40% of those are for generics. That’s 17.3 hours a week for one clinic - nearly half a full-time employee’s work - just on paperwork.
One Reddit user, a healthcare provider, wrote: “My clinic spends 17.3 hours weekly just on prior auths for generics - that’s nearly half a full-time employee’s time on administrative work instead of patient care.” That’s not efficiency. That’s waste.
What You Can Do
You’re not powerless. Here’s how to protect yourself:
- Ask before your prescription is filled. When your doctor writes a new script, ask: “Is this generic going to need prior authorization?” If yes, find out what’s needed so they can start the process right away.
- Keep records. Save every email, phone log, and denial letter. The Crohn’s & Colitis Foundation found that 67% of prior auth denials for generics can be reversed with better documentation.
- Request urgent review. If you’re on a medication that affects your health daily - like insulin, thyroid meds, or blood pressure pills - ask your doctor to mark the request as urgent. Cigna and others are required to respond in 72 hours for urgent cases.
- Call your insurer. Don’t wait for the pharmacy to tell you. Log into your insurance portal or call customer service. Ask: “Is generic [drug name] covered without prior authorization?” Sometimes the pharmacy doesn’t know the full details.
- Ask about alternatives. If your generic is blocked, ask your doctor: “Is there another generic in the same class that’s approved?” Sometimes switching to a different brand of the same drug type bypasses the block.

The Bigger Picture
Generics were supposed to be the solution - not the problem. They’re 80-90% cheaper than brand-name drugs. They’re just as safe. They’re the reason millions of Americans can afford their meds. But when insurers start treating them like high-risk specialty drugs, they’re not saving money - they’re costing the system more.
A 2025 statement from the American Gastroenterological Association found that prior authorization for first-line generics increases total healthcare costs by 18% because of delayed treatment, ER visits, and hospitalizations. That’s the opposite of what these systems were designed to do.
It’s like locking the door to the cheapest room in the hotel and making guests fill out forms just to get in. The goal was to reduce waste. Instead, it’s creating more.
Reforms are coming. States are acting. Insurers are backing down - slowly. But until the system fully recognizes that generics are not the problem, patients will keep paying the price - in time, stress, and health.
What’s Next?
The Congressional Budget Office projects a 40% drop in prior authorization for generics by 2028 - if current reforms keep moving. That’s good news. But until then, the burden stays on patients and providers.
If you’re on a generic medication and suddenly can’t get it, you’re not alone. And you’re not crazy. This isn’t how it was supposed to work. But now that it’s happening, knowing how to fight it - and when to push back - is your best tool.
Why would insurance require prior authorization for a generic drug?
Even though generics are cheaper, insurers sometimes require prior authorization to control which specific version of a drug you get - often because they get higher rebates from one manufacturer over another. It’s also used to enforce step therapy, where you must try one generic before moving to another, even if both are equally effective. This isn’t about safety - it’s about formulary management and profit.
Which generic drugs are most likely to need prior authorization?
Oncology generics, like methotrexate or capecitabine, have the highest rates - up to 35% require approval. Other common targets include certain thyroid medications, immunosuppressants for autoimmune conditions, and some antidepressants. But increasingly, even routine drugs like metformin, lisinopril, and levothyroxine are being flagged, especially in private insurance plans.
How long does prior authorization for generics usually take?
For standard requests, it can take 5-10 business days. For urgent cases - like if you’re at risk of hospitalization or your condition is worsening - insurers must respond within 72 hours under federal rules for Medicare Advantage and many state laws. But in practice, delays still happen, especially if the provider’s office doesn’t submit electronically.
Can I appeal a denial for a generic drug?
Yes, and you should. About 67% of prior authorization denials for generics are overturned on appeal, especially if your doctor provides updated clinical notes, lab results, or evidence that other generics failed or aren’t appropriate. Always keep copies of every communication and ask your doctor to help you file the appeal.
Are there any generics that can’t be blocked by prior authorization?
In some states, yes. California’s Essential Drug List includes 47 common generics - like metformin, levothyroxine, and amoxicillin - that insurers can no longer require prior authorization for as of January 2025. Medicaid programs in 34 states also restrict prior authorization for certain generic classes. And starting in 2026, Medicare Advantage plans must follow federal rules that limit these barriers.




Comments (10)
Jenna Allison
Just had this happen with my mom’s metoprolol. Pharmacy said ‘prior auth required’ - she’s 72, on fixed income, and this pill keeps her out of the hospital. Took 6 days to get approved. Her doctor had to call twice, fax paperwork, and then the insurer lost it. This isn’t healthcare. It’s bureaucratic torture.
Vatsal Patel
Oh wow. So the system designed to save money now costs you time, stress, and possibly your life? Genius. Truly. The only thing more efficient than this process is the PBM’s quarterly bonus. Maybe next they’ll make you fill out a form to breathe air. Free market at work, folks.
Helen Leite
THEY’RE DOING THIS ON PURPOSE 😱💸 I I know it!! PBMs are in bed with Big Pharma and they’re making us suffer so they can profit from the *expensive* versions!! It’s not a glitch - it’s a CONSPIRACY!! 🕵️♀️💊 #PriorAuthIsEvil #GenericsAreBeingHijacked
Shanta Blank
Let me get this straight - we’ve got a system where the cheapest option gets treated like a high-security narcotic? The only thing more absurd is how everyone acts surprised. This is capitalism with the brakes off. They don’t care if you die, they care if your insurer’s rebate check clears. And doctors? They’re just the clerks now. Welcome to 2026, where your health is a spreadsheet.
Tiffany Wagner
i just got my lisinopril approved after 8 days. my doc submitted it on day one. i keep forgetting to follow up because i’m so tired of fighting. why does this have to be so hard
Amelia Williams
Don’t give up. I was in the same boat last year with my metformin. Called my insurer, found out they were pushing a different generic with a higher rebate. I asked my doctor to switch - boom, no auth needed. It’s annoying, but you *can* outmaneuver the system. Keep pushing. Your health matters more than their formulary.
Sharon Biggins
my drs office told me to call the pharmacy back and ask for the formulary code. i did and they said oh its covered no auth needed. turns out the pharmacy just messed up the code. sometimes its not the insurer its the tech. dont stress too much yet. just ask
Michael Camilleri
People complain about prior auth for generics like it's new. It's not. It's just the natural evolution of profit over people. You think your doctor cares? They're drowning in paperwork. You think the insurer cares? Their job is to deny, not to heal. This isn't broken. It's working exactly as designed. You're just not the customer. You're the cost center.
lorraine england
My sister’s pharmacist actually called her to say ‘we’re gonna fight this for you’ - and they did! Took 4 days. She’s on levothyroxine. No one should have to beg for a pill that’s been around since the 80s. But hey, at least some places still have human beings working there. Hold onto those pharmacies.
Himanshu Singh
It's like asking for water from a faucet that only opens if you write a poem about the rain. We've turned healthcare into a ritual of suffering. Generics were meant to be the bridge - now they're the obstacle. Maybe the real problem isn't the system. Maybe it's that we accepted it as normal.