
Before you start a new medication, especially one that treats serious conditions, you need to ask: Is there a REMS program? REMS stands for Risk Evaluation and Mitigation Strategy. It’s not just a paperwork hurdle-it’s a safety system built by the U.S. Food and Drug Administration (FDA) to make sure high-risk drugs don’t cause more harm than good. If your doctor prescribes a drug with a REMS program, skipping the steps could mean delayed treatment, denied refills, or even dangerous side effects. You’re not alone if this feels confusing. Thousands of patients and providers face the same challenge every day.
What Exactly Is a REMS Program?
REMS programs were created after the FDA gained authority under the Food and Drug Administration Amendments Act of 2007. They’re required for medications with serious safety risks-like birth defects, life-threatening infections, addiction, or sudden death-that can’t be managed with standard warnings alone. As of early 2026, there are 76 active REMS programs in the U.S. These aren’t optional. If your drug has one, you must follow it to get the prescription filled.
Not all REMS are the same. Some just give you a printed Medication Guide. Others demand much more. For example:
- Zyprexa Relprevv (for schizophrenia) can only be given in certified clinics, and you must be monitored for at least three hours after each injection.
- iPLEDGE (for isotretinoin, used for severe acne) requires both you and your doctor to register online, take pregnancy tests monthly, and use two forms of birth control if you’re female.
- Thalidomide (used for multiple myeloma) requires prescriber certification, patient enrollment, and mandatory contraception for both men and women.
- Opioid painkillers require prescriber education but no certification or registry-just proof you’ve completed a training course.
These aren’t arbitrary rules. They’re based on real harm. Isotretinoin caused thousands of birth defects before iPLEDGE started. Thalidomide led to severe limb deformities in the 1950s. REMS exists to prevent history from repeating itself.
How to Find Out If Your Medication Has a REMS Program
Don’t wait for your pharmacist to tell you. Start checking before your first prescription.
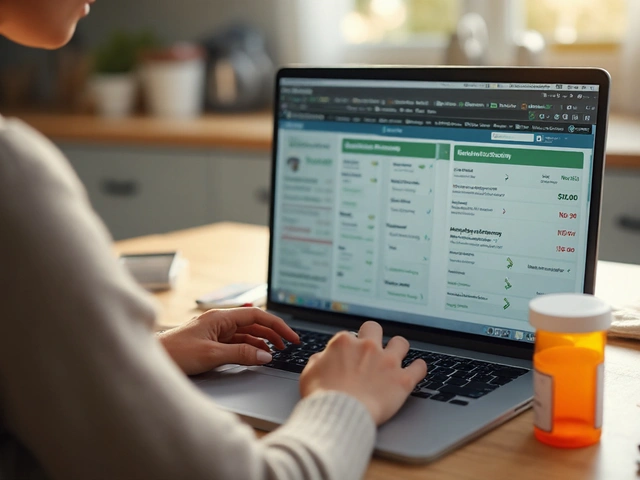
Step 1: Look at the prescribing information. Every FDA-approved drug has a full prescribing document called the “Package Insert.” It’s available on DailyMed (dailymed.nlm.nih.gov). Search your drug name. If there’s a REMS, it will say so clearly under the “REMS” section. If you see phrases like “requires certification,” “patient registry,” or “restricted distribution,” you’re dealing with a REMS.
Step 2: Use the FDA’s REMS Public Dashboard. This free, updated tool (fda.gov/drugs/risk-evaluation-and-mitigation-strategies-rems) lets you search by drug name, company, or REMS type. It shows you exactly what’s required-whether it’s training, monitoring, or special dispensing rules. The dashboard was upgraded in March 2023 to show real-time updates, though delays of up to two weeks can still happen.
Step 3: Check the manufacturer’s website. Most drugmakers have a dedicated REMS section. For example:
- iPLEDGE: ileDGEprogram.com
- Thalidomide: celgene.com/rems
- Mycophenolate: mycophenolaterems.com
These sites have enrollment forms, training videos, and contact numbers. Don’t ignore them. Many patients miss their refills because they didn’t know they had to re-enroll every year.
Who’s Responsible for Making Sure REMS Are Followed?
It’s not just the doctor’s job. It’s a team effort.
Prescribers must be certified or trained before they can write the prescription. For drugs like thalidomide or Zyprexa Relprevv, they need to log into the REMS portal, complete training, and get a unique ID. Without that ID, pharmacies won’t fill the script.
Pharmacists are the final gatekeepers. They check for:
- Prescriber certification status
- Patient enrollment in registries
- Valid pregnancy test dates (for teratogenic drugs)
- Proof of completed education
One hospital pharmacy in Texas cut isotretinoin processing time from 45 minutes to 15 minutes by creating a checklist. They print it out and verify each box before handing over the bottle.
Patients need to know their role too. If your drug requires you to register, sign up. If you need a blood test or pregnancy test, get it done. If you miss a step, your refill will be denied. And yes, this can delay treatment. A 2022 survey found 42% of patients on REMS drugs waited an average of 6.2 business days just to get started.

What Happens If You Skip a REMS Step?
Nothing good.
Pharmacies are legally required to refuse to dispense REMS drugs if requirements aren’t met. That means:
- Your prescription sits in the system, waiting.
- You may need to call your doctor to re-certify.
- You might have to schedule an appointment just to get a pregnancy test or complete training.
Some patients try to get around this by switching pharmacies or asking for “just one dose.” That doesn’t work. REMS systems are linked across pharmacies. If you’re not enrolled, no pharmacy can legally give you the drug.
And it’s not just about refills. If you take a REMS drug without following the rules and have a bad reaction, your insurance may refuse to pay. In rare cases, providers can face fines or lose their license for non-compliance.
How Much Time Should You Plan for REMS Verification?
Don’t assume this will take five minutes. It can take hours-or even days.
For most drugs with simple Medication Guides, you’re fine. But for those with Elements to Assure Safe Use (ETASU), here’s what to expect:
- Prescriber certification: 60-90 minutes of training, plus filling out forms. Can take 3-7 days to process.
- Patient enrollment: 15-30 minutes online, but may require ID verification or faxing documents.
- Lab testing: Scheduling, waiting for results, and sending them to the REMS program can add 2-5 days.
- Specialized administration: You may need to travel to a certified clinic and block off 3-4 hours for monitoring.
The American Society of Health-System Pharmacists recommends setting aside 8-12 minutes per REMS drug during your initial consultation. But that’s just for the doctor’s side. Patients should budget extra time for their own steps.
What to Do If You’re Delayed or Confused
If you’re stuck, don’t panic. Here’s what works:
- Contact the pharmacy. They often have REMS coordinators who know the exact steps. Ask: “What do I need to do for this REMS?”
- Call the manufacturer’s REMS help line. Most have a toll-free number listed on their REMS website. They can walk you through enrollment.
- Ask your doctor’s office for a REMS checklist. Many clinics now print one out for patients.
- Use the CME Passport tool. If your drug requires continuing education (like opioids or mycophenolate), this site finds accredited courses you can take online.
Don’t rely on Google searches. REMS rules change. Always go to official sources: FDA, manufacturer, or pharmacy.
Why REMS Programs Are Still Necessary-Even If They’re Frustrating
Yes, REMS adds steps. Yes, it’s time-consuming. A 2019 survey found 68% of doctors say REMS slows down care. But here’s the truth: without REMS, some of these drugs wouldn’t be available at all.
Dr. Robert Epstein, former FDA deputy director, put it simply: “REMS enables the FDA to approve, and patients to have access to, certain drugs with risks that would otherwise exceed their benefits.”
Think of it this way: Thalidomide was pulled from the market in 1962 after causing 10,000+ birth defects worldwide. Today, it’s used to treat cancer-because REMS makes it safe enough to use. Isotretinoin is still the most effective acne treatment ever made, but only because iPLEDGE prevents fetal exposure.
REMS isn’t perfect. The FDA has modified 37% of programs since 2015 to reduce burden. New rules in 2023 require patient-friendly apps and electronic verification. By 2026, blockchain may even be used to track certifications securely.
But right now? You still have to do the steps. There’s no shortcut.
Quick Checklist: REMS Verification Before Starting a Medication
Before you take your first dose, confirm these five things:
- Check the drug’s prescribing info on DailyMed for “REMS” in the header.
- Search the FDA REMS Public Dashboard to confirm active requirements.
- Visit the manufacturer’s REMS website and read all patient instructions.
- Ask your doctor: “Do I need to be certified? Do I need to enroll?”
- Call your pharmacy and ask: “What paperwork do I need to bring?”
If you’re unsure about any step, don’t guess. Call someone who knows. The risk isn’t worth it.
What’s Coming Next in REMS?
REMS is evolving. By 2026, expect:
- More programs for gene therapies and biologics-up to 90% of new cancer drugs will need them.
- Electronic integration: Your EHR system may auto-check REMS status when your doctor writes the script.
- Mobile apps: FDA now requires all new REMS to include smartphone tools for patient reminders and verification.
- Reduced paperwork: The FDA’s 2023 Modernization Initiative has already cut 30-40% of redundant steps in 14 programs.
But until then-stay proactive. REMS isn’t going away. It’s getting smarter. Your job? Stay informed, stay organized, and never assume someone else will handle it for you.
How do I know if my medication has a REMS program?
Check the drug’s prescribing information on DailyMed (dailymed.nlm.nih.gov) or search the FDA’s REMS Public Dashboard. If a REMS is required, it will be clearly labeled. You can also call your pharmacist or check the manufacturer’s website-most have a dedicated REMS section with enrollment details.
Can I get a REMS drug without completing the requirements?
No. Pharmacies are legally required to refuse to dispense REMS drugs if the safety requirements aren’t met. This includes missing prescriber certification, unverified pregnancy tests, or lack of patient enrollment. Skipping steps means your prescription won’t be filled, no matter how urgent your need.
How long does REMS verification usually take?
It varies. Simple Medication Guides take minutes. Programs requiring prescriber certification or patient enrollment can take 3-7 days. Lab testing and clinic visits may add another 2-5 days. Plan ahead-don’t wait until your last pill is gone.
Do I need to repeat REMS steps for refills?
Yes, for most programs. Some require annual re-enrollment, monthly pregnancy tests, or yearly training updates. Always check the REMS program rules for renewal timelines. Your pharmacy will remind you, but don’t rely on it-keep your own records.
What if my doctor doesn’t know about the REMS?
Ask them to check the FDA REMS Public Dashboard or the manufacturer’s website. Many providers aren’t fully aware of every REMS, especially for newer drugs. Bring printed instructions or the REMS website link to your appointment. You’re your own best advocate.



Comments (14)
Ian Detrick
REMS feels like a bureaucratic maze, but honestly? It’s the only thing standing between me and another thalidomide disaster. I get why it’s annoying-waiting weeks for a script-but I’d rather wait than have my kid born with no arms. We’ve seen what happens when we don’t do this right.
Shruti Badhwar
As a healthcare professional in India, I find REMS systems both admirable and impractical in resource-limited settings. While the intent is noble, the infrastructure required for certification, registries, and lab tracking simply doesn’t exist in many regions. This creates a dangerous disparity: patients in high-income countries get access with bureaucracy; those elsewhere get none at all.
Liam Tanner
For anyone new to this: don’t stress. I used to panic every time my doctor prescribed something new. Now I just open DailyMed before the appointment. If I see ‘REMS’ in the header, I print the page and bring it to the pharmacy. Took me three tries to get it right, but now it’s routine. You got this.
Ian Ring
Okay, I’ll admit-I rolled my eyes at REMS at first. But then my cousin got prescribed isotretinoin, and I watched the whole iPLEDGE process: registration, two forms of birth control, monthly labs, mandatory counseling… it was insane. But? She’s acne-free, and her sister’s baby is healthy. So… yeah. Maybe it’s not perfect, but it’s necessary. 🙏
Angela Goree
Why are we letting Big Pharma dictate how we treat patients? This whole REMS system is just a way for drug companies to charge more and control distribution. They profit from the paperwork, the clinics, the certifications. It’s not safety-it’s profit with a badge.
Shanahan Crowell
Big respect to the pharmacists who handle this. My local pharmacy has a REMS coordinator who texts me reminders, prints checklists, and even calls my doctor if something’s stuck. I used to think I was the only one struggling-turns out, they’re the real MVPs.
Kerry Howarth
Check DailyMed first. Always. It’s free, official, and updated within 48 hours. No guesswork. No third-party blogs. Just the facts.
Tiffany Channell
People complain about REMS like it’s a personal attack. Meanwhile, 10,000 babies were born deformed because no one cared enough to regulate thalidomide. You want convenience? Then accept that some risks aren’t worth taking. Stop whining and do the paperwork.
Neela Sharma
REMS isn’t bureaucracy-it’s a lifeline woven in red tape. Like a temple gate that only opens when you’ve washed your hands, said your prayer, and left your ego at the door. The drug doesn’t care if you’re rushed. The body remembers what the system forgets. So pause. Breathe. Register. You’re not just following rules-you’re honoring life.
Michael Burgess
Just got my first REMS script (opiate for chronic pain) and it was smoother than expected. Used the CME Passport app to finish the training in 20 mins on my phone. The pharmacy sent me a reminder text 3 days before my refill was due. Honestly? Feels like tech is finally catching up. Still annoying, but less like a nightmare.
Hank Pannell
From a pharmacoeconomic standpoint, REMS represents a classic risk-benefit optimization framework under the FDA’s post-marketing surveillance mandate. The ETASU components-prescriber certification, patient enrollment, and restricted distribution-function as non-pharmacological risk mitigation interventions that attenuate adverse event incidence while preserving therapeutic access. The 2023 Modernization Initiative’s reduction in redundant steps reflects a shift toward dynamic, data-driven REMS design, leveraging EHR integration and blockchain-based verification to reduce administrative burden while maintaining safety integrity. Still, the lag between regulatory updates and real-world implementation remains a systemic bottleneck.
Wren Hamley
REMS is just a fancy way of saying ‘we messed up before, so now we’re gonna make you jump through hoops.’ But hey, if it stops another thalidomide? Fine. I’ll do the forms. Just don’t make me call three different places to prove I’m not pregnant. That’s ridiculous.
veronica guillen giles
Oh wow, you actually read the whole thing? Congrats. You’re now one of the 3% of patients who didn’t just take the pill and hope for the best. The rest of us? We’re still Googling ‘is this drug going to turn me into a zombie?’ and praying to the pharmacy gods.
Tru Vista
REMS? Yeah I know about it. You just go to the website. It’s easy. Everyone else is just lazy. My doctor didn’t even know about it-so I told him. He was impressed. I’m basically a healthcare superhero now.